More than 40% of adults taking prescription or over-the-counter medications are at risk of dangerous interactions with alcohol-yet most don’t know it. You might think having a glass of wine with your painkiller or a beer after your antibiotic is harmless. But the truth is, mixing alcohol with even common medications can lead to dizziness, liver failure, breathing problems, or worse. This isn’t theory. It’s happening every day in homes, emergency rooms, and hospitals across the country.
How Alcohol Changes How Your Medications Work
Alcohol doesn’t just make you feel drunk-it changes how your body handles medicine. Your liver uses special enzymes, like CYP2E1 and CYP3A4, to break down both alcohol and most medications. When you drink, these enzymes get overwhelmed. That means your medication either stays in your system too long-or doesn’t work at all.
There are two main ways this happens:
- Pharmacokinetic interactions: Alcohol blocks or speeds up how your liver processes the drug. If it blocks it, your medication builds up to dangerous levels. If it speeds it up, the drug stops working. For example, drinking while taking acetaminophen (Tylenol) can cause your liver to produce a toxic byproduct that leads to sudden liver failure-even if you’ve never had liver problems before.
- Pharmacodynamic interactions: Alcohol and your medication hit the same part of your brain or body. Think of it like two people pushing the same brake pedal. Benzodiazepines like Xanax or Valium already slow your nervous system down. Add alcohol, and that slowdown becomes extreme. At just 0.05% blood alcohol (about one drink), this combo can cause dangerous breathing problems.
Medications That Are Especially Dangerous with Alcohol
Not all meds react the same way. Some are low risk. Others? One drink can land you in the ER.
1. Antibiotics Like Metronidazole (Flagyl)
This one catches people off guard. Metronidazole fights infections, but if you drink even a small amount-like a sip of wine or a beer-you’ll likely get a reaction called disulfiram-like syndrome. Symptoms include: flushing, pounding heart, nausea, vomiting, and chest pain. In 92% of cases, this happens with just one drink. There’s no safe amount. Doctors say: no alcohol for at least 72 hours before and after taking it.
2. Benzodiazepines and Sleep Aids
Medications like diazepam (Valium), alprazolam (Xanax), and zolpidem (Ambien) are central nervous system depressants. Alcohol does the same thing. Together, they can slow your breathing to a deadly level. Studies show this combo increases GABA receptor activity by 400%. That’s why it’s responsible for 32% of all alcohol-medication deaths. Even if you’ve taken these meds for years, adding alcohol makes them far more dangerous.
3. Opioids and Painkillers
Morphine, oxycodone, hydrocodone-any opioid combined with alcohol increases the risk of respiratory failure by up to 8 times. The CDC says this is one of the top causes of accidental overdose deaths. You don’t need to get drunk. Even one drink can tip the balance.
4. Antidepressants (SSRIs)
Fluoxetine (Prozac), sertraline (Zoloft), and others may seem safe, but alcohol can make depression worse and increase side effects like drowsiness, dizziness, and impaired judgment. One study found alcohol stays in your system 3.2 hours longer when taken with SSRIs. That means you feel drunk longer-and your mood may dip further.
5. Over-the-Counter Drugs
You don’t need a prescription to be at risk.
- Acetaminophen (Tylenol): Taking more than three drinks a day while using Tylenol can cause acute liver failure. Even moderate drinking (one or two drinks daily) can raise liver enzyme levels in nearly half of users.
- NSAIDs (ibuprofen, naproxen): These can cause stomach bleeding, especially when combined with alcohol. The risk goes up by 300-500%.
- Antihistamines (Benadryl): These make you sleepy. Alcohol makes it worse-up to 300% more drowsiness. That’s dangerous if you need to drive or operate machinery.
Who’s Most at Risk?
It’s not just older adults or heavy drinkers. The biggest group at risk? People between 40 and 59 who take multiple medications. Here’s why:
- Aging bodies: After age 65, liver blood flow drops by about 35%. That means alcohol and meds stick around longer, increasing side effects.
- Multiple prescriptions: Nearly 70% of seniors take five or more meds. Each one adds another chance for a bad interaction.
- Hidden risks: Many people don’t realize their cold medicine, allergy pill, or sleep aid contains alcohol or interacts with it.
The American Geriatrics Society lists 17 medications with high-risk alcohol interactions specifically for older adults. If you’re over 65 and drink-even occasionally-you need to know which ones you’re taking.
What You Can Do to Stay Safe
You don’t have to give up alcohol forever. But you do need to be smart.
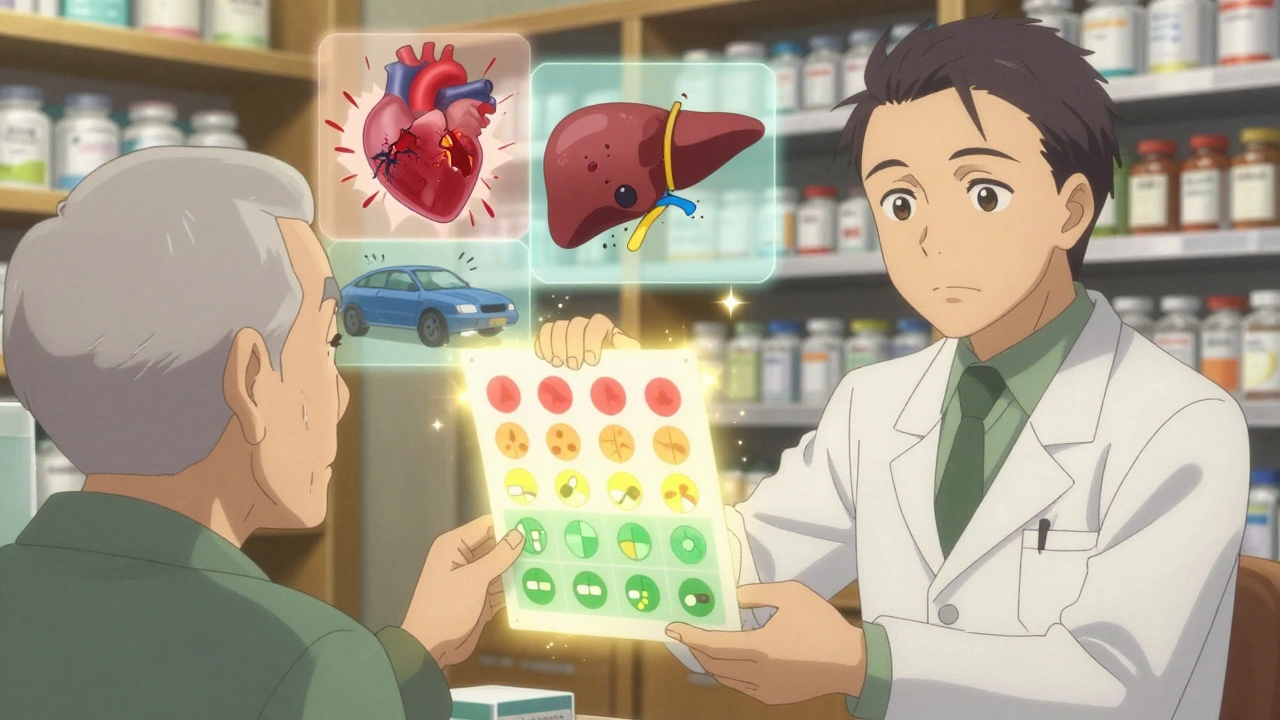
1. Ask Your Doctor or Pharmacist
Don’t assume your prescriber knows you drink. Only 32% of doctors routinely ask about alcohol use during appointments. When you get a new prescription, ask: “Is it safe to drink alcohol with this?” If they don’t know, ask for a pharmacist to review your full list.
2. Know Your Standard Drink
A “drink” isn’t what you think.
- 12 oz beer (5% alcohol)
- 5 oz wine (12% alcohol)
- 1.5 oz distilled spirits (40% alcohol)
Most people pour way more than this at home. Use a measuring cup if you’re unsure.
3. Wait 2-3 Hours After Taking Your Med
If your doctor says it’s okay to drink occasionally, wait at least two to three hours after taking your medication. That gives your body time to absorb and start processing it before alcohol enters the mix.
4. Never Drink on an Empty Stomach
Eating before drinking slows alcohol absorption by 25-30%. It won’t stop the interaction-but it can reduce how fast it hits you.
5. Use a Trusted Interaction Checker
WebMD and GoodRx have free tools. But be careful: a 2022 study found only 37% of online checkers reflect current FDA guidelines. Stick to ones linked to hospitals or government sites.
What to Do If You’ve Already Mixed Them
If you’ve accidentally combined alcohol with a risky medication and feel:
- Extreme drowsiness or confusion
- Difficulty breathing
- Fast heartbeat or chest pain
- Severe nausea or vomiting
Call 911 or go to the nearest emergency room. Don’t wait. Don’t try to “sleep it off.” This isn’t a hangover. This is a medical emergency.
Why Warning Labels Often Fail
You might think your prescription bottle says “Do not drink alcohol.” But here’s the truth: only 42% of prescription bottles in the U.S. include a clear alcohol warning, according to a 2021 FDA audit. Many labels say “avoid alcohol” without explaining why-or how dangerous it really is.
That’s why patient education matters more than ever. A 2023 study showed that when pharmacists gave patients a simple color-coded chart showing which meds were high-risk, understanding jumped from 48% to 82%. Visuals work. Simple language works. Repeating the warning works.
The Bigger Picture
This isn’t just about one person making a bad choice. It’s a system-wide problem. Four out of five adults take at least one medication. More than half of those over 65 take five or more. Alcohol is everywhere-in social events, family dinners, weekend routines. And the medical system hasn’t kept up.
New FDA rules starting in 2024 require clearer warning labels on high-risk medications. Telehealth platforms are now screening patients for alcohol use before prescribing. Pharmacies are training staff to flag interactions automatically.
But none of that matters if you don’t know what to look for.
Final Advice: When in Doubt, Skip It
If you’re unsure whether your medication is safe with alcohol-don’t take the chance. The risks aren’t theoretical. They’re documented. They’re measured. They’re deadly.
There’s no such thing as “just one drink” with metronidazole, opioids, or benzodiazepines. There’s no safe gray area with acetaminophen if you drink daily. And if you’re over 65, your body doesn’t handle the combo like it used to.
Ask questions. Read labels. Talk to your pharmacist. Keep a list of all your meds-and the alcohol warnings that come with them.
Your liver, your brain, and your life depend on it.
Can I have one drink with my prescription?
It depends on the medication. For antibiotics like metronidazole, opioids, or benzodiazepines-no. Even one drink can be dangerous. For some antidepressants or NSAIDs, occasional light drinking might be okay-but only if your doctor says so. Always ask first. Never guess.
How long should I wait after taking medication before drinking alcohol?
For most medications, wait at least 2-3 hours after your dose. But for drugs with long half-lives like diazepam (Valium), which stays in your system for days, you need to avoid alcohol for 5-10 days after your last dose. For metronidazole, avoid alcohol for 72 hours before and after treatment. Check your specific medication’s half-life or ask your pharmacist.
Is it safe to drink alcohol with over-the-counter meds like Tylenol or ibuprofen?
Tylenol (acetaminophen) and alcohol together can cause liver damage-even with moderate drinking. Avoid alcohol entirely if you take Tylenol regularly. Ibuprofen and alcohol increase your risk of stomach bleeding by 300-500%. If you drink often, skip NSAIDs. Use acetaminophen only occasionally and never with more than one drink.
Why don’t doctors always warn me about alcohol interactions?
Many doctors don’t ask about alcohol use during appointments. A 2022 survey found 68% of patients were never warned about alcohol-medication risks by their prescriber. It’s not always negligence-time is short, and alcohol isn’t always part of the conversation. That’s why you need to bring it up yourself.
Can I drink alcohol the day after taking a medication?
It depends on how long the drug stays in your system. For short-acting drugs like amoxicillin, one drink the next day is usually fine. But for long-acting drugs like fluoxetine (Prozac) or diazepam (Valium), the drug can still be active 2-5 days after your last dose. Check the half-life or ask your pharmacist. When in doubt, wait 72 hours.
What should I do if I accidentally mixed alcohol and medication?
If you feel dizzy, nauseous, confused, have trouble breathing, or your heart races-call 911 immediately. Don’t wait. Don’t try to drive yourself. These reactions can escalate quickly. If symptoms are mild, call your pharmacist or poison control (1-800-222-1222 in the U.S.) for advice. But never assume it’s “just a hangover.”





Shayne Smith
December 7 2025I had no idea mixing wine with my ibuprofen could wreck my stomach like that. I always thought it was just a myth. Thanks for laying this out so clearly.
Priya Ranjan
December 7 2025People still drink with meds? This isn’t 1998. If you can’t follow basic safety rules, you’re not just risking your life-you’re wasting medical resources. Stop being irresponsible.
Kumar Shubhranshu
December 7 2025Metronidazole and alcohol is a hard no. One sip and you’re on the floor. Seen it happen. No excuses.
Nava Jothy
December 9 2025I mean... it’s almost poetic how we’ve built a society that normalizes self-destruction. One drink to unwind... then another to numb the anxiety caused by the first drink... then a pill to sleep... then another drink to forget the pill... we’re all just ghosts in a pharmacological maze. 💔🍷
brenda olvera
December 10 2025This is so important i wish every pharmacy had a little card like this taped to the counter i feel like we all need a reminder now and then
Myles White
December 12 2025I’ve been on SSRIs for six years and I’ve had one glass of wine with dinner maybe twice a month. My doctor said it’s fine as long as I don’t binge. But I didn’t know alcohol sticks around longer when you’re on them-that’s wild. I’m going to cut back even more now. Also, the part about Tylenol and liver failure? Scary. I used to take two every night for back pain. I’m switching to heat packs now. Thanks for the wake-up call.
olive ashley
December 14 2025You know what’s really dangerous? The fact that the FDA only started requiring clearer labels in 2024. That’s 70 years too late. Big Pharma knew. Doctors knew. Pharmacies knew. But they didn’t want you to stop drinking. They want you to keep buying meds. And now you’re supposed to trust a 37% accurate online checker? Please. The system is rigged. Don’t believe the labels. Believe your gut. And if you’re over 65? Don’t trust anyone. Not even your pharmacist.
Annie Gardiner
December 14 2025I get it, alcohol’s bad with meds. But honestly? I think the real problem is that we’ve turned everything into a moral panic. People just want to relax. You don’t need to scare them into sobriety. Maybe instead of listing every possible death scenario, we could say: ‘If you’re unsure, skip it.’ That’s enough. Less fear. More trust. We’re adults.