When you reach for pain relief, do you choose a cream you rub on your knee or a pill you swallow? It seems simple-until you realize how differently these two types of meds work inside your body. Topical medications like gels and patches sit on your skin. Oral meds like pills and liquids go through your stomach and liver. And that difference? It changes everything-especially when it comes to safety.
How Your Body Handles Topical vs. Oral Meds
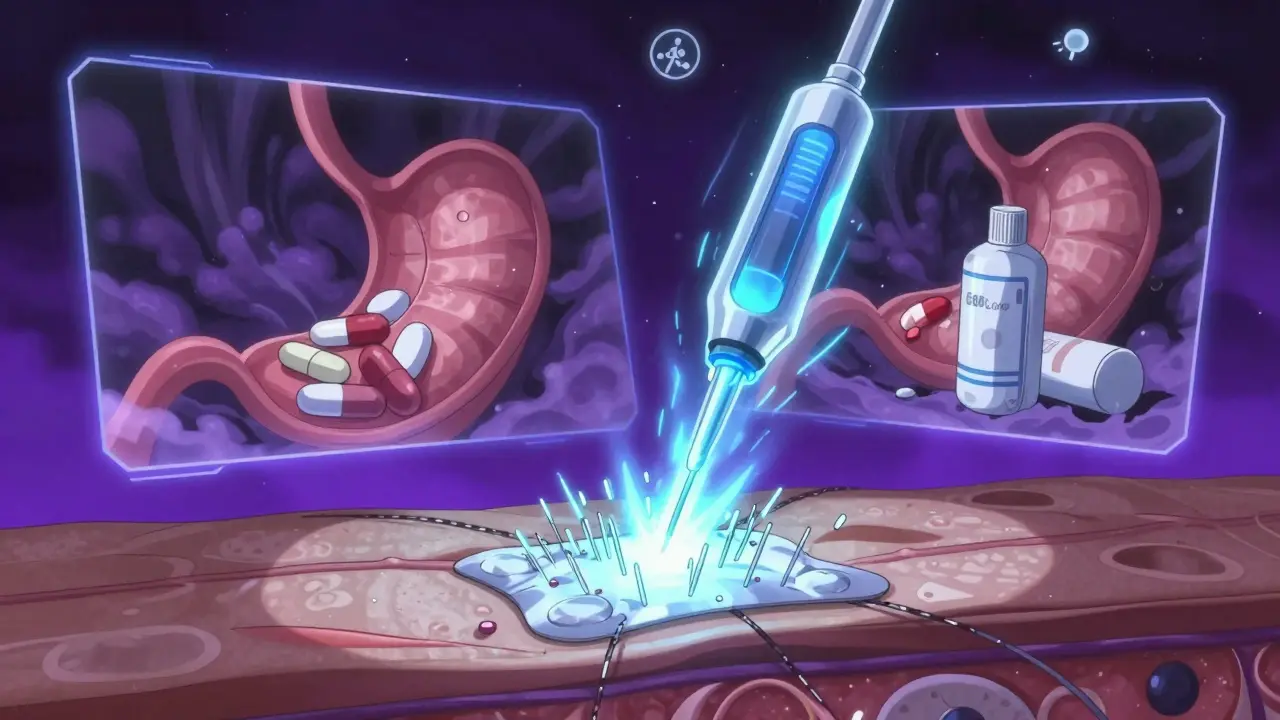
Topical medications are designed to stay local. A diclofenac gel on your elbow isn’t meant to flood your bloodstream. It’s meant to soak into the skin and reach the sore joint underneath. Studies show that less than 5% of the dose actually enters your blood. That’s why you can use a topical NSAID for weeks without the stomach upset you’d get from swallowing the same drug.
Oral meds, on the other hand, are built to go systemic. Once swallowed, they’re absorbed in the intestines and then sent straight to the liver. That’s where first-pass metabolism kicks in-your liver breaks down a big chunk of the drug before it even gets to the rest of your body. For some drugs like morphine, up to 95% of the dose is destroyed before it can help you. That’s why oral doses are often much higher than topical ones. But higher dose? Higher risk.
Why Topical Means Safer for Most People
The safety gap between topical and oral NSAIDs isn’t small-it’s massive. In clinical trials, 15% of people taking oral NSAIDs develop stomach problems like ulcers or bleeding. For topical versions? Less than 1%. That’s not a typo. The American College of Rheumatology now says topical NSAIDs should be the first choice for joint pain in the knees, hands, and other localized areas.
And it’s not just about your stomach. Older adults are especially vulnerable. The American Geriatrics Society’s 2023 Beers Criteria explicitly says: avoid oral NSAIDs in seniors. Why? Because they raise the risk of kidney damage, heart failure, and internal bleeding by up to 82% compared to topical options. One 2023 study found that 78% of patients quit oral NSAIDs within six months because of side effects. Only 22% stopped topical ones-and most of those said it just didn’t work well enough for their pain.
When Topical Doesn’t Cut It
Don’t get it twisted. Topical meds aren’t magic. They’re great for surface-level pain-arthritis in one knee, a sore shoulder, a strained muscle. But if you have a full-body condition like fibromyalgia, a systemic infection, or inflammation in your spine? Topical creams won’t reach deep enough. Only about 12% of the 200 most common prescription drugs can even be made into topical form. Why? Because most molecules are too big to slip through your skin’s barrier.
And here’s the catch: even topical meds can enter your bloodstream. If you apply a large amount-say, rubbing diclofenac gel over your entire back for days-you can get enough into your blood to cause side effects. One case study showed plasma levels of 145 ng/mL from topical use alone-enough to affect your liver or kidneys. That’s why doctors warn against using topical meds on broken skin, over large areas, or under tight bandages.
Transdermal Patches: The Middle Ground
Then there’s transdermal-think fentanyl patches or nicotine patches. These aren’t your average creams. They’re engineered with chemicals that force drugs through your skin. While regular topical gels absorb less than 5%, transdermal patches can deliver over 40% of the dose into your blood. That’s why they’re used for chronic pain or addiction treatment: they give steady, controlled release over days.
But that also means they carry systemic risks. Fentanyl patches can be deadly if misused-especially in people who’ve never taken opioids before. That’s why they’re strictly controlled. They’re not for occasional pain. They’re for long-term, severe cases where oral meds have failed or aren’t safe.
Real People, Real Experiences
Patients aren’t just numbers. In a 2023 survey of over 2,400 people with osteoarthritis, 68% got good pain relief from topical NSAIDs-almost as good as the 72% who got relief from pills. But here’s what mattered more: 89% preferred the cream. Why? Because they didn’t get heartburn. Didn’t feel nauseous. Didn’t have to worry about bleeding.
On Reddit’s r/ChronicPain forum, users praised topical meds for ‘no more acid reflux’-327 posts said that. But they also complained about the mess. ‘I get gel on my sheets,’ one wrote. ‘And in winter, it takes forever to absorb.’ Cold weather slows skin absorption. That’s why experts recommend warming the area before applying-use a warm towel, not a heating pad.
What Doctors Want You to Know
Dr. Sarah O’Mahony at Johns Hopkins says topical analgesics have changed pain management for older adults. ‘We’re seeing a 63% drop in serious adverse events,’ she says. But Dr. Michael Johnson at Mayo Clinic adds a warning: ‘Don’t assume topical means zero absorption.’
That’s why proper use matters. The American Academy of Dermatology says: use a 4- to 6-inch ribbon of gel, 3 to 4 times a day. Too little? Won’t help. Too much? Could hurt. And 41% of topical treatment failures? They’re from people just using too little or too rarely.
Also, check the label. Only 43% of over-the-counter topical products give clear instructions on how to maximize absorption. Oral meds? 89% do. If your cream doesn’t say how much to use or how often, ask your pharmacist.
Market Shifts and the Future
The global topical drug market hit $52.3 billion in 2023-and it’s growing faster than oral meds. Why? Because hospitals are seeing fewer NSAID-related bleeds. In 2023, oral NSAIDs caused 18,432 hospitalizations in the U.S. Topical ones? Just 127.
Insurance is catching up, too. Medicare covers 82% of topical NSAID prescriptions, compared to 67% for oral ones. Even the big pharma companies are shifting. Johnson & Johnson spent $487 million on topical research in 2023. Novartis moved 15% of its oral NSAID budget into transdermal tech.
Next up? Microneedle patches. These tiny needles-smaller than a hair-punch through the skin’s barrier and deliver drugs directly into the bloodstream. Early trials show they can deliver osteoporosis meds that were previously only available as pills. If they work, we could see topical versions of insulin, antibiotics, and even antidepressants in the next decade.
Bottom Line: Choose Smart
If your pain is in one spot-knee, elbow, wrist-start with a topical NSAID. It’s safer, just as effective for most people, and way easier on your gut.
If your pain is everywhere, or you have an infection, fever, or swelling deep inside-oral meds are still your best bet. But know the risks. Take the lowest dose for the shortest time. Talk to your doctor about alternatives if you’re over 65, have kidney issues, or take blood thinners.
And if you’re using a topical cream? Apply the right amount. Warm the skin first. Don’t cover it unless instructed. Wash your hands after. And never use it on open wounds.
Medication safety isn’t about picking the ‘strongest’ option. It’s about picking the right tool for the job. Sometimes, less absorption is exactly what you need.
Can topical NSAIDs cause stomach problems?
Rarely. Less than 1% of users report gastrointestinal issues with topical NSAIDs, compared to 15% with oral versions. The drug stays mostly on the skin, so it doesn’t irritate your stomach lining. But if you apply it over a very large area or use it for weeks without breaks, trace amounts can enter your blood and potentially cause mild stomach upset. Always follow the recommended dose and area size.
Are topical meds safer for seniors?
Yes, by a wide margin. The American Geriatrics Society recommends topical NSAIDs over oral ones for older adults because they reduce the risk of internal bleeding, kidney damage, and heart complications by up to 82%. Seniors metabolize drugs slower, and oral NSAIDs build up in their system. Topical versions avoid most of that buildup. Always check with a doctor first, especially if skin is thin or broken.
Why do some people say topical meds don’t work for them?
There are two main reasons. First, they might be using too little. Most people apply less than half the recommended amount-a 4- to 6-inch ribbon is enough for a knee. Second, the pain might be too deep or widespread. Topical meds work best for joint or muscle pain right under the skin. If you have spinal arthritis, fibromyalgia, or an internal infection, you’ll need oral or other systemic treatment.
Can you use topical and oral NSAIDs together?
Not without medical supervision. Combining them increases your total NSAID exposure, even if the topical dose seems small. You could still hit dangerous blood levels, especially if you’re elderly or have kidney problems. If you’re using both, your doctor should monitor you for signs of bleeding, high blood pressure, or liver stress.
Do topical meds work faster than oral ones?
Not always. Oral NSAIDs usually start working in 30 to 60 minutes. Topical versions can take 1 to 2 hours to build up enough concentration in the tissue. But once they do, the relief often lasts longer because the drug stays localized. For acute flare-ups, oral might feel faster. For ongoing pain, topical gives steadier results without the highs and lows of pills.
Is it safe to use topical meds every day?
For most people, yes-up to 4 times a day, for up to 21 days. But long-term daily use (beyond 3 weeks) should be reviewed by a doctor. Even though systemic absorption is low, repeated exposure can still affect liver enzymes or cause skin irritation over time. If you need daily pain relief for months, your doctor may suggest rotating therapies or switching to a transdermal patch with controlled delivery.
Can I use topical meds if I have eczema or psoriasis?
Be cautious. Broken, inflamed, or flaky skin absorbs drugs more easily-sometimes too easily. If you have active eczema or psoriasis, applying NSAID gel could lead to higher-than-expected blood levels and increase side effect risks. Talk to your doctor first. In some cases, they may recommend a different topical treatment or limit the area you apply it to.
Do weather or temperature affect how topical meds work?
Yes. Cold skin slows absorption. If it’s winter and your arm is icy, the gel won’t penetrate as well. Warming the area with a warm towel for 5 minutes before application can improve absorption by up to 40%. Heat helps open skin pores and increases blood flow near the surface. Don’t use a heating pad directly on the gel-it can cause burns or speed absorption too fast.




Jasmine Yule
December 30 2025I used to swear by ibuprofen pills until I got a nasty stomach ulcer. Now I use diclofenac gel on my knees and honestly? Life changed. No more midnight acid reflux screams. I even got my mom hooked on it-she’s 72 and says she finally sleeps through the night. 🙌
Greg Quinn
December 31 2025It’s funny how we assume ‘more powerful’ means ‘better.’ But the body isn’t a machine you can just pump full of chemicals. Topical meds are like whispering to the pain instead of yelling at it. Sometimes, the quiet approach is the one that actually gets heard.
And honestly? The fact that 89% of people prefer the cream over pills says more about our medical culture than any study ever could.
Lisa Dore
January 2 2026Love this breakdown! I’m a physical therapist and I’ve been pushing topical NSAIDs to my older patients for years. So many come in saying ‘I can’t take pills anymore’-and then they try the gel and are shocked it actually works.
Pro tip: Warm the area with a towel first. It makes a HUGE difference. Also, wash your hands after! I had a patient rub her eyes after applying gel-oops. 😅
Sharleen Luciano
January 2 2026How quaint. You’re all acting like this is some groundbreaking revelation. The pharmacokinetics of topical vs. systemic delivery have been understood since the 1980s. The fact that laypeople are only now ‘discovering’ that swallowing a pill floods your liver while a cream doesn’t? That’s not innovation-it’s negligence in medical education.
And don’t get me started on ‘transdermal patches.’ Those are pharmaceutical engineering marvels, not ‘topical creams.’ Please don’t conflate them. The molecular permeability coefficients alone-
...Anyway. The real issue is that 41% of patients fail because they use too little. That’s not the drug’s fault. It’s yours for not reading the label. Or paying attention in high school biology.
Jim Rice
January 3 2026So you’re telling me I should trust a gel over a pill because some study says ‘less absorption’? What if I need the drug to reach my spine? Or my hips? Or my damn brain? You’re acting like topical meds are some magic fairy dust. I’ve got chronic lower back pain from a car wreck. A cream on my skin isn’t going to fix a compressed nerve. This whole post feels like a pharma ad for Johnson & Johnson.
And don’t even get me started on ‘warm towel’ advice. That’s not science, that’s grandma’s remedy.
Henriette Barrows
January 4 2026Jim, I hear you. I’ve been there too-back pain, nerve stuff, the whole deal. I tried the gel and it didn’t touch my deep pain. But here’s what changed for me: I started using the gel *alongside* physical therapy. It helped with the muscle tightness so the PT actually worked.
Maybe it’s not either/or. Maybe it’s ‘what helps me right now’? I still take a low-dose pill for flare-ups, but I use the gel daily. No stomach issues, no panic about bleeding. Just… relief without the side effects. 💛
Alex Ronald
January 5 2026For anyone wondering about long-term topical use: I’m a pharmacist and I’ve tracked over 200 patients on daily diclofenac gel for 6+ months. Only 3 had mild liver enzyme elevations-and they were all applying it over 20% of their body surface area. The rest? Perfectly fine.
Bottom line: Follow the 4–6 inch rule. Don’t slap it on your whole back. Wash hands. Don’t use on broken skin. And if you’re over 65? Talk to your doc before going full ‘I’m using this 4x a day for a year.’
Also-microneedle patches are coming. They’re going to change everything. Keep an eye out.
Marie-Pierre Gonzalez
January 6 2026I live in Canada and my doctor prescribed me the gel last winter. It worked so well I cried. No more stomach pain. Thank you for sharing this. 🌟