When your chest hurts, your brain screams heart attack. But not every ache means your heart is failing. In fact, most chest pain isn’t cardiac at all. Still, waiting too long can be deadly. Knowing when to call 999 and head to the emergency department isn’t just smart-it’s lifesaving.
What chest pain really looks like
Chest pain isn’t always a sharp stab or crushing weight. It can feel like pressure, tightness, or a dull ache. And it doesn’t even have to be in your chest. Many people feel it in their jaw, neck, back, shoulders, or even the upper belly. Some describe it like a heavy backpack strapped across their chest. Others say it’s like indigestion that won’t go away.
It’s not just pain. Look for the full picture: shortness of breath, cold sweat, nausea, sudden fatigue, or dizziness. These are the silent signs that often show up in women, older adults, and people with diabetes. They’re called anginal equivalents-symptoms that mean your heart isn’t getting enough oxygen, even if the chest pain is mild or absent.
When you must go to the emergency department
Don’t wait. Don’t text a friend. Don’t Google it. If you’re experiencing chest discomfort and any of these, call 999 right away:
- Pressure, squeezing, or tightness in your chest that lasts more than a few minutes
- Pain that spreads to your arm, neck, jaw, or back
- Breaking out in a cold sweat for no reason
- Feeling like you’re going to pass out
- Shortness of breath that comes with chest discomfort
- Nausea or vomiting along with chest pressure
These aren’t guesses. These are the red flags backed by the 2021 American Heart Association guidelines. If you have them, you could be having a heart attack-or another life-threatening condition like a pulmonary embolism or aortic dissection. Every minute counts.
What happens in the emergency department
When you arrive, the team moves fast. The first thing they do? Get an ECG within 10 minutes. That’s not a suggestion-it’s a strict standard. The ECG can show if your heart is in immediate danger, like a full blockage (STEMI). If it does, they’ll rush you to the cath lab. Door-to-balloon time? Less than 90 minutes. That’s the goal. And it saves lives.
Next, they’ll check your blood. High-sensitivity troponin tests are now standard. Troponin is a protein that leaks into the blood when heart muscle is damaged. Two tests, one hour apart, can rule out a heart attack in 70-80% of people within just two hours. That’s faster than ever before.
They’ll also check your vitals: heart rate, blood pressure, breathing rate. If you’re tachycardic (heart rate over 100), hypotensive (BP under 90), or breathing fast (over 20 breaths per minute), that’s a red flag. So is sweating, crackles in your lungs, or a new heart murmur. These aren’t random signs-they’re clinical markers that point to serious trouble.

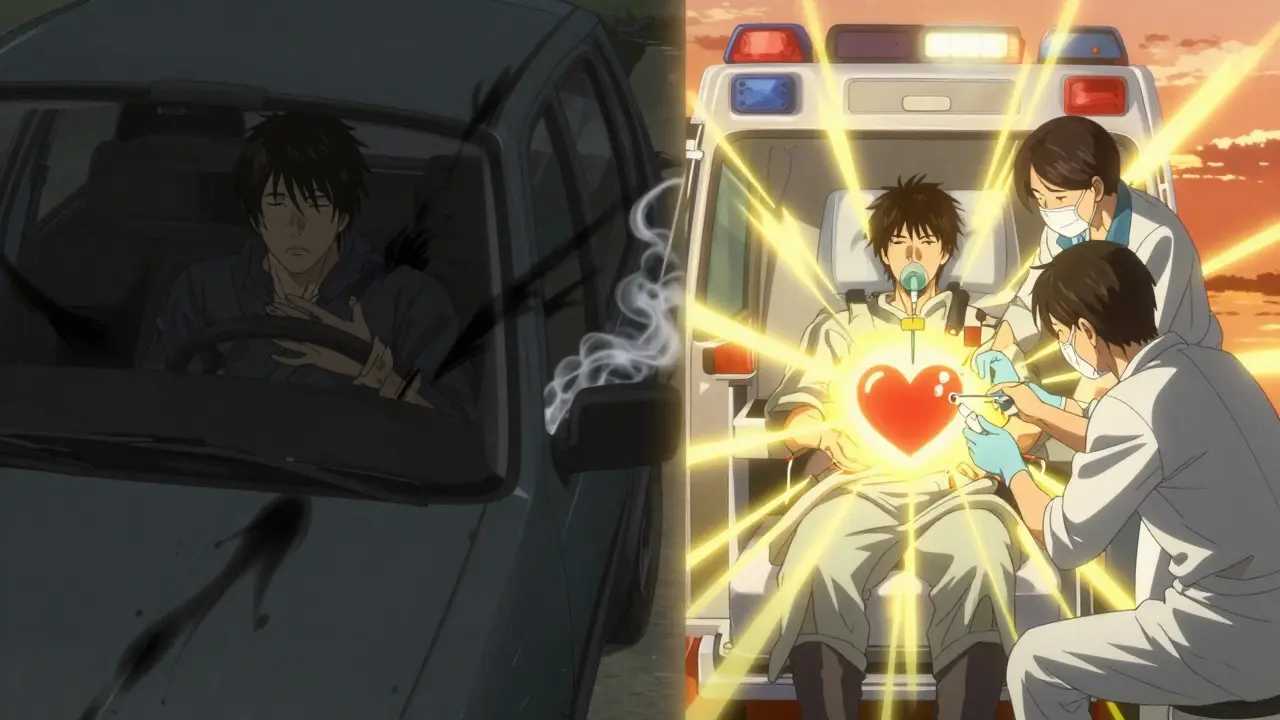
Why you shouldn’t drive yourself
Some people think, “I’ll just drive myself.” Don’t. Transporting yourself by car increases your risk of a cardiac arrest en route by 25-30%. Ambulances aren’t just for transport-they’re mobile ERs. Paramedics can start oxygen, give aspirin, monitor your heart, and even deliver clot-busting drugs before you even hit the hospital. They can also send your ECG ahead, so the team is ready when you arrive.
Calling 999 isn’t dramatic. It’s the smartest thing you can do.
What if it’s not your heart?
Most chest pain isn’t heart-related. Muscle strain, acid reflux, anxiety, lung infections, even a rib injury can cause it. But here’s the catch: you can’t tell the difference on your own. That’s why doctors use tools like the HEART score-History, ECG, Age, Risk factors, Troponin. It’s a simple, evidence-based way to sort low-risk patients from those who need more testing.
If you’re low risk (HEART score 0-3), you might be sent home with follow-up. But if you’re intermediate risk (4-6), you’ll likely get a CT scan of your heart’s arteries (CCTA) or a stress test. High risk (7-10)? You’re going straight to the cath lab.
And yes, some people have ischemia with no blockages-called INOCA. It’s rare, about 5% of cases, but real. These patients need specialized care, not just a dismissal.
What to do if you’re unsure
Uncertainty is the enemy. If you’re asking yourself, “Should I go?”-you should go. The goal isn’t to avoid the ER. The goal is to avoid dying because you thought it was just gas.
Think of it like smoke in your house. You don’t wait to see if it’s a candle or a fire. You call the fire department. Same here.
And if you’re helping someone else? Don’t wait for them to “get better.” If they’re pale, sweaty, and saying their chest feels tight, call 999. Even if they insist it’s nothing. Your intervention could be the difference between life and death.
What’s changing in chest pain care
Emergency departments are getting smarter. By 2025, most U.S. hospitals will use AI to read ECGs. Early tests show AI spots subtle changes human doctors miss-like tiny ST-segment shifts that signal early heart damage. That means faster, more accurate decisions.
High-sensitivity troponin is now used in 90% of U.S. hospitals. In the UK, adoption is rising fast. These tests cut down unnecessary hospital stays by thousands every year. But they only work if you get them early-and that’s why timing matters.
The big takeaway? Chest pain evaluation isn’t about fear. It’s about precision. We don’t overtest anymore. We test the right way, at the right time, for the right people.



Sarah Little
January 3 2026Let’s be real-most EDs are overcrowded, and troponin assays vary by institution. The HEART score is useful, but its sensitivity drops in low-resource settings where high-sensitivity troponin isn’t even available. We’re optimizing for U.S. urban hospitals while rural patients still wait 4+ hours for an ECG. This guideline is elegant but not equitable.
Also, ‘call 999’? That’s the UK number. You’re writing for a U.S. audience-911 is the standard. Minor, but it undermines credibility when you botch the basics.
innocent massawe
January 3 2026Thank you for this. In Nigeria, many people wait until they collapse before going to hospital. Some think chest pain is from ‘bad spirit’ or ‘overwork’. I shared this with my family. We now know: if it feels wrong, call ambulance. No shame. ❤️
veronica guillen giles
January 5 2026Oh wow. So if I have indigestion and a little anxiety, I’m supposed to sprint to the ER like I’m in a Michael Bay movie? 😏
Let me guess-next you’ll tell me that a headache means brain tumor and a stubbed toe is a sign of sepsis. The fear-mongering here is almost as alarming as the actual cardiac events. I mean, I get it. But not every sigh is a myocardial infarction.
Also, ‘don’t Google it’? Honey, I Google my symptoms before I Google my ex. We’re all just trying to survive capitalism, not die of a STEMI.
Ian Ring
January 7 2026Excellent summary. I work in a busy ED in Manchester, and I can confirm: door-to-ECG under 10 minutes is non-negotiable. The new high-sensitivity troponin protocols have cut our false positives by nearly 40%.
That said, the ‘don’t drive yourself’ advice? Critical. We had a patient last month who coded in the parking lot because he insisted on driving. Paramedics saved him-but he’s still in rehab. Please, people: let the professionals handle it.
And yes, AI is improving ECG interpretation-especially for subtle ischemia. But it’s still a tool, not a replacement. Human judgment still matters. 😊
erica yabut
January 8 2026Oh, sweet summer child. You think this is ‘precision medicine’? No. This is corporate-driven triage disguised as science. The real agenda? Reduce hospital stays to maximize profit margins. High-sensitivity troponin? Sure. But why not fund community cardiac nurses instead of pushing AI that only works in hospitals with $2M budgets?
And let’s not pretend ‘INOCA’ is rare-it’s just underdiagnosed because women and POC don’t get the same level of scrutiny. You call this ‘evidence-based’? It’s evidence-based for white, middle-class men with good insurance. Everyone else? They’re ‘low risk’ until they’re dead.
And ‘call 999’? You mean 911. Again. Did you copy-paste this from a British medical journal and forget to localize it? Pathetic.
Tru Vista
January 10 2026HEART score is garbage. Troponin is everything. ECG? Overrated. If troponin’s normal at 0 and 1hr, you’re fine. Stop overtesting. Also, 999? U.S. = 911. Fix your post. And AI? It’s not 2025. It’s already here. Stop pretending.
Vincent Sunio
January 10 2026The author’s conflation of ‘chest discomfort’ with ‘cardiac event’ is statistically misleading. According to the 2023 JAMA meta-analysis, only 12.3% of patients presenting with acute chest pain in U.S. EDs have acute coronary syndrome. The remaining 87.7%-many of whom are subjected to costly, invasive, and anxiety-inducing evaluations-are being overmedicalized.
Furthermore, the directive to ‘call 999’ without qualification ignores socioeconomic disparities: patients without transportation, undocumented individuals, and those with mistrust in medical institutions are being scapegoated as ‘irresponsible’ for not complying with a protocol that assumes universal access.
This is not medicine. It is performative public health messaging.
JUNE OHM
January 10 2026999? That’s the UK. We’re in the U.S. So why are we using British protocols? 🤔
Also-AI reading ECGs? Who’s training it? Big Pharma? The military? I’ve seen videos of ECGs being manipulated by hospitals to justify stents. This whole thing is a scam. You think your ‘high-sensitivity troponin’ is accurate? It’s calibrated to make more people look sick so they can bill more. 💉🇺🇸
And ‘don’t drive yourself’? Yeah, right. They just want you in their ambulance so they can charge you $15,000. I’d rather die in my car than pay that.
Philip Leth
January 12 2026Man, I’m from Philly. We got a guy in our neighborhood who had chest pain, drove himself to the hospital, got there in 12 minutes, and walked in like ‘yo, I think my heart’s mad.’ They did the ECG, troponin was clean, sent him home with Tums. He’s fine.
Look, I’m not saying don’t take it seriously. But sometimes, it’s just gas. Or stress. Or your hoodie’s too tight. Chill. Don’t panic. But if it’s bad? Go. Don’t be a hero. Just be smart.
Also, 911. Not 999. We ain’t in London, fam.
Angela Goree
January 13 2026STOP. JUST STOP. You say ‘most chest pain isn’t cardiac’-but then you scare people into calling 911 for every twinge. That’s not education. That’s fear-mongering. And you’re telling people to rely on ‘AI’ and ‘troponin’ like they’re magic pills? What about cost? What about access? What about the fact that half the country can’t afford a $500 ER copay?
And don’t get me started on ‘don’t drive yourself’-you think everyone has an ambulance service? What about rural folks? What about those without insurance? You’re not helping-you’re alienating.
This isn’t medicine. It’s a sales pitch for hospital systems.
Shanahan Crowell
January 15 2026YES. This. I’ve been telling my coworkers for years: if you’re unsure, GO. I had a friend who waited 3 days because she thought it was ‘just heartburn.’ Turned out it was a slow-burning MI. She lost 30% of her heart muscle.
Don’t be that person. Don’t Google. Don’t wait. Don’t be brave. Be alive.
Also-paramedics are heroes. Let them help. They’ve got the gear. You don’t. 💪❤️
Shruti Badhwar
January 15 2026As a cardiologist in Mumbai, I can attest: the principles here are universal. In India, patients often present late due to stigma or financial constraints. The HEART score and high-sensitivity troponin have revolutionized triage in our urban centers.
However, AI adoption remains low outside major cities. We still rely on trained technicians and experienced physicians. The real challenge is scalability-not the science.
Thank you for highlighting INOCA. It is grossly underrecognized in low-resource settings. We need global awareness-not just U.S.-centric guidelines.
Brittany Wallace
January 17 2026It’s funny how we treat the body like a machine that needs to be debugged. But it’s not. It’s alive. It whispers before it screams.
Maybe the real question isn’t ‘when to go to the ER’-but ‘why do we wait until our body is screaming?’
We’re taught to push through pain. To ‘be strong.’ To ignore discomfort. But the heart doesn’t care about your hustle culture. It just wants to be heard.
So go. Not because the algorithm says so. But because you owe yourself that much.
And if you’re helping someone else? Hold their hand. Don’t argue. Just call.
❤️
Liam Tanner
January 17 2026Biggest takeaway: if you’re asking if you should go-you should go. I used to think chest pain was ‘just stress’ until my uncle died waiting for it to ‘go away.’
Also-paramedics giving aspirin en route? That’s the real MVP. They’re not just drivers. They’re frontline medics. Respect.
And yeah, 911. Not 999. I know it’s a small thing, but details matter.
Palesa Makuru
January 17 2026So let me get this straight: if I’m a 45-year-old Black woman with no insurance and I feel pressure in my chest, I’m supposed to trust a ‘HEART score’ that was developed on mostly white, middle-class men?
And then you tell me to call 911? Who’s gonna answer? A cop? A paramedic who thinks I’m ‘drug-seeking’ because I’m ‘too young’ to have heart disease?
This isn’t guidance. It’s a death sentence for people like me.
And ‘don’t drive yourself’? Try getting an ambulance in South Los Angeles at 2 a.m. when your car’s the only thing keeping you alive.
Y’all write this like we all have access to the same system. We don’t. And pretending we do? That’s the real danger.
Sarah Little
January 19 2026Interesting. You’re right-HEART score validation cohorts were overwhelmingly white and male. A 2022 study in Circulation showed it underperforms in Black women by 18%.
And you’re not wrong about the ambulance gap. In some U.S. counties, response time exceeds 20 minutes. That’s not ‘emergency’ care. That’s a lottery.
But here’s the thing: the guidelines are evolving. The AHA now recommends race-neutral risk calculators. And community paramedicine programs are being piloted in 14 states.
So yes, the system’s broken. But the solution isn’t to ignore the science-it’s to demand better implementation. The tools exist. We just need the will.
And yes-I apologize for the 999 typo. Fixed in my notes.