Obesity Medication Dosing Calculator
Obesity affects drug distribution and metabolism. Standard doses based on total body weight (TBW) may be ineffective or dangerous.
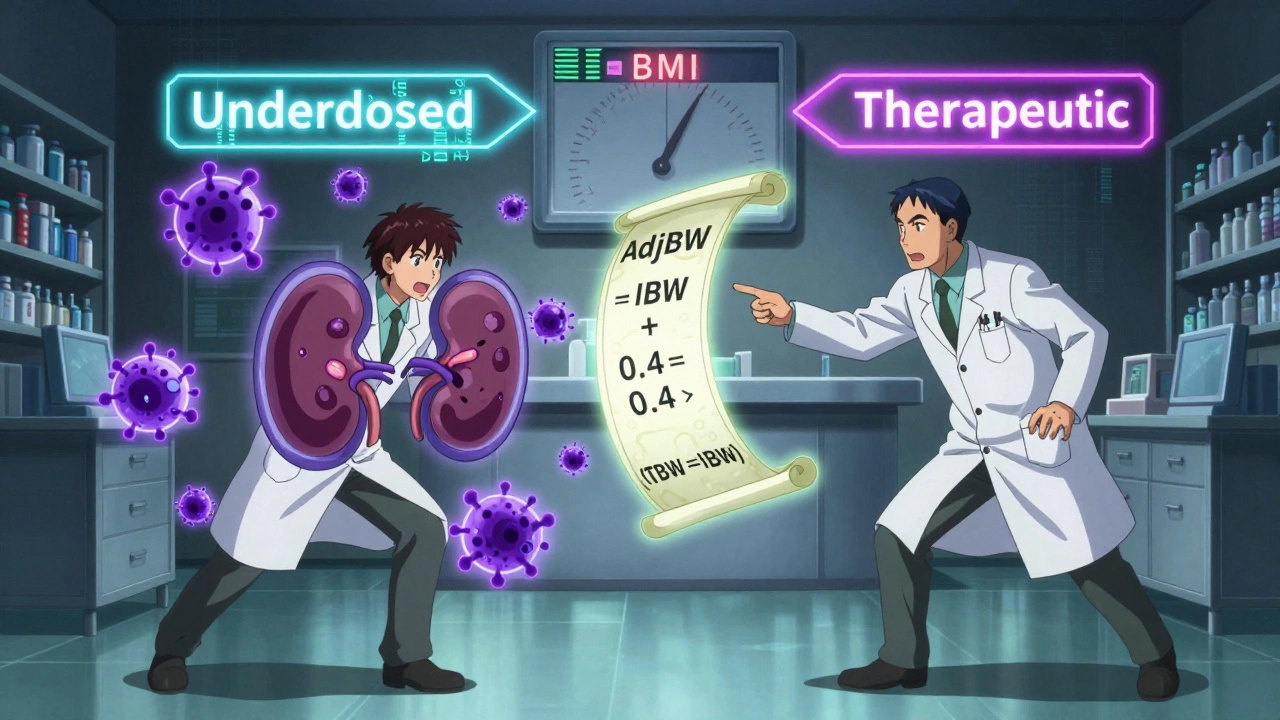
This calculator determines your Adjusted Body Weight (AdjBW), which is the recommended metric for many antibiotics and other medications in obese patients. AdjBW is calculated as:
AdjBW = IBW + 0.4 × (TBW − IBW)
Your Calculated Weight Metrics
Why Adjusted Body Weight Matters
For antibiotics like ceftriaxone, using TBW (140 kg) could lead to treatment failure in 63% of obese patients. Using AdjBW (103 kg) ensures therapeutic levels.
The UCSF protocol recommends 2g daily for BMI >30, not the standard 1g dose.
Example from article: 140 kg patient at 5'10" has IBW of 78 kg, AdjBW of 103 kg
This is why the 2023 UCSF protocol recommends higher ceftriaxone dosing for obese patients.
Why standard drug doses don’t work for people with obesity
When a doctor prescribes a pill, they usually think in terms of a standard dose - 500 mg of amoxicillin, 10 mg of warfarin, 40 mg of enoxaparin. But for someone with obesity, that same dose might be too weak, too strong, or just plain useless. It’s not about how much you weigh on the scale. It’s about what’s inside that weight.
Obesity changes how your body handles medicine. More fat means drugs move differently, break down differently, and stick around longer or shorter than expected. The result? You could be getting a dose that’s too low to fight an infection, or too high and risking kidney damage. Studies show 21% to 37% of obese patients on standard doses experience treatment failure - meaning their infection doesn’t clear, their blood clot isn’t prevented, or their pain isn’t controlled.
How fat changes the way drugs work in your body
Your body isn’t just a bag of water and muscle. Fat tissue behaves like a sponge for some drugs and a wall for others. Lipophilic drugs - ones that dissolve in fat - like diazepam or fluoxetine, soak into fat stores. In a person with Class III obesity (BMI ≥40), the volume of distribution for these drugs can more than double. That means the drug gets spread out so thin that it never reaches the concentration needed to work.
On the flip side, hydrophilic drugs - water-soluble ones like antibiotics such as cephazolin or vancomycin - don’t mix well with fat. They stay in your blood and fluid spaces. But obesity increases your total blood volume and kidney function. That means these drugs get cleared faster. A standard 1g dose of ceftriaxone might drop below therapeutic levels in 63% of obese patients within hours. Meanwhile, a normal-weight person might still have enough drug in their system to kill bacteria.
Protein binding also shifts. Many drugs cling to proteins in the blood. In obesity, those proteins can be altered or diluted, leaving more free drug floating around - which can lead to unexpected side effects even when the total dose looks right.
What weight should doctors use to calculate your dose?
It’s not as simple as using your total body weight. Here are the three key measurements doctors and pharmacists now use:
- Total Body Weight (TBW): Your actual weight on the scale. Often too high for water-soluble drugs, too low for fat-soluble ones.
- Ideal Body Weight (IBW): A calculated estimate of what your weight should be based on height and gender. For men: 50 kg + 2.3 kg for every inch over 5 feet. For women: 45.5 kg + 2.3 kg per inch over 5 feet.
- Adjusted Body Weight (AdjBW): A hybrid. It’s IBW plus 40% of the difference between your TBW and IBW. Formula: AdjBW = IBW + 0.4 × (TBW − IBW). This is the go-to for most antibiotics in obese patients.
- Lean Body Weight (LBW): Estimates muscle and organ mass, excluding fat. Used for drugs like beta-blockers or anticoagulants where fat doesn’t play a big role.
For example, if you weigh 140 kg (308 lbs) and are 5’10”, your IBW is about 78 kg. Your AdjBW would be 78 + 0.4 × (140 − 78) = 103 kg. That’s the number used to calculate your dose of ceftriaxone - not your full 140 kg.
Antibiotics: Where dosing mistakes are most dangerous
Antibiotics are where the stakes are highest. A wrong dose in an obese patient can mean a lingering infection, sepsis, or even death.
Take ceftriaxone. Standard dose: 1g daily. In obese patients? That dose fails in over half the cases. The 2023 UCSF protocol now recommends a minimum of 2g daily for BMI >30. At Stanford Health Care, switching to this dose dropped surgical site infections from 14.2% to 8.7% in over 1,200 patients.
Colistin is another example. It’s a last-resort antibiotic, but it’s toxic to kidneys. Dosing by total weight can lead to 44% kidney damage in obese patients. The IDSA recommends capping the daily dose at 360 mg of colistin base activity - based on IBW, not TBW.
Tigecycline is different. It’s dosed the same regardless of weight: 100 mg loading, then 50 mg every 12 hours. But new 2024 data suggests for resistant infections, doubling the dose to 200 mg loading and 100 mg maintenance may be needed - even in very obese patients.
Anticoagulants: The 85 kg tipping point
Apixaban, a blood thinner, has a dangerous cutoff: 85 kg. Below that, 5 mg twice daily. Above it? 10 mg twice daily. But here’s the problem - that’s not based on science. It’s based on a single trial that grouped patients at 85 kg. People just under 85 kg get half the dose of those just over. That creates a 100% jump in exposure. Medicare data shows 47% higher bleeding risk in patients just above the threshold.
Enoxaparin (Lovenox) is even trickier. For BMI 40-49.9, 40 mg twice daily is standard. For BMI ≥50? You need 60 mg twice daily. One study found 21% of obese patients on 40 mg had subtherapeutic anti-Xa levels - meaning no protection against clots. A 2018 JAMA Surgery trial showed 40 mg reduced clots by 37% compared to 20 mg - but only if the patient’s BMI was under 50.
Therapeutic Drug Monitoring: The missing safety net
Many drugs don’t have clear dosing rules for obesity. That’s where Therapeutic Drug Monitoring (TDM) comes in. TDM means taking a blood sample to measure exactly how much drug is in your system. It’s not just for ICU patients anymore.
The Infectious Diseases Society of America (IDSA) strongly recommends TDM for vancomycin, aminoglycosides, and voriconazole in obese patients. Stanford’s 2022 study found that when they switched from total weight to adjusted weight dosing for voriconazole, supratherapeutic levels dropped from 39% to 12%. That’s a 70% reduction in overdose risk.
But only 37% of U.S. hospitals have formal obesity dosing protocols. And only 63% of pharmacists say their institutions support TDM programs. That means a lot of patients are getting doses based on guesswork.
What’s being done to fix this?
The problem is growing. Over 39% of U.S. adults are obese - and that number keeps rising. The FDA now requires drug companies to include obese patients in clinical trials, especially those with BMI ≥50. In 2024, they expanded that requirement to make sure trials include enough data on the heaviest patients.
Tools are improving too. DoseMe, a Bayesian dosing software, is now used by 83% of U.S. academic medical centers. It uses your weight, kidney function, and blood levels to predict the perfect dose. Lexidrug and MediCalc offer calculators for IBW and AdjBW. The Obesity Medicine Association runs quarterly webinars on dosing. And in 2023, the NIH gave $4.7 million to track how obesity affects drug levels over time in 500 patients.
Still, only 0.7% of NIH-funded pharmacokinetic studies since 2015 focused on obesity. That’s a huge gap. The White House’s 2024 National Strategy now allocates $28 million specifically for obesity medication research - a sign that change is finally coming.
What you can do as a patient
If you have obesity and are on any medication - especially antibiotics, blood thinners, or psychiatric drugs - ask these questions:
- Is my dose based on my total weight, or my adjusted/ideal weight?
- Has my doctor considered my BMI when prescribing this?
- Could therapeutic drug monitoring help me?
- Is there a more precise dosing guideline for this drug in obese patients?
Don’t assume your doctor knows. A 2021 University of Michigan study found 43% of internal medicine residents were confused about when to use total weight vs. adjusted weight. That’s not incompetence - it’s a system failure. You have the right to ask for evidence-based dosing.
The bottom line
Obesity isn’t just a number on a scale. It’s a biological shift that changes how your body absorbs, moves, and gets rid of medicine. Standard doses are designed for the average person - not for someone with 100 extra pounds of fat. Using total body weight for all drugs is outdated and dangerous. Adjusted body weight, lean body weight, and therapeutic drug monitoring aren’t optional extras - they’re essential tools.
The science is clear. The guidelines exist. The tools are available. What’s missing is consistent application. Until every hospital, every pharmacist, and every prescriber uses the right weight metric for the right drug, patients with obesity will keep getting underdosed, overdosed, or left with treatment failures. You deserve better. And you have the right to demand it.

Shannon Gabrielle
December 1 2025So let me get this straight-we’re telling doctors to guess at doses because the FDA didn’t care enough to test on fat people until 2024? Classic. We’re not patients. We’re lab rats with extra padding.
Dennis Jesuyon Balogun
December 2 2025The pharmacokinetic paradigm is fundamentally anthropocentric-designed for the normative, the lean, the statistically average. Obesity isn't a comorbidity; it's a systemic perturbation of volume distribution, protein binding, and clearance kinetics. We're applying Newtonian models to relativistic physiology. The result? Therapeutic nihilism disguised as protocol.
Grant Hurley
December 4 2025I had a friend on vancomycin and they kept getting sick even though the doc said "it’s the right dose." Turns out they used total weight. She was on 2g daily but her levels were garbage. Once they switched to adjusted weight? She bounced back in 48 hours. Why isn’t this common knowledge??
Kshitij Shah
December 5 2025In India we call this "doctor ka formula"-they give the same pill to everyone. My uncle, 130 kg, got the same amoxicillin as my 60 kg cousin. He got sepsis. They blamed his "bad lifestyle." Not the dose. Classic.
soorya Raju
December 5 2025this is all a big pharma scam to sell more drugs. they dont want you to get better they want you to keep buying. the real cure is fasting and juicing. the FDA is in bed with the pharmaceutical cartel. they dont want you to know that vitamin c cures everything. they just want your money.
Lucinda Bresnehan
December 6 2025I’m a pharmacist and I’ve seen this over and over. A 160 kg patient on enoxaparin gets 40 mg because that’s what the system auto-populates. They don’t even check BMI. I’ve had to manually override 12 times this month. It’s not just negligence-it’s systemic laziness. We need mandatory EHR prompts for adjusted dosing.
ANN JACOBS
December 6 2025It is, without a shadow of a doubt, a profound and deeply concerning failure of our modern medical infrastructure that the physiological realities of adipose tissue have been so systematically ignored in pharmacological modeling. The implications for patient safety, healthcare equity, and clinical outcomes are not merely statistical-they are existential. We are, in effect, prescribing by proxy, using a model designed for a demographic that no longer constitutes the majority. This is not just an oversight; it is a moral lapse.
Nnaemeka Kingsley
December 7 2025man i never thought about this. my cousin lost her leg to an infection because the antibiotics didn’t work. they just kept giving her the same dose. i told her to ask about her weight but she was too scared. yall need to make this info easier for normal folks to understand.
Sean McCarthy
December 7 2025This is why we need mandatory obesity pharmacology certification for all prescribers. No more guessing. No more "it’s close enough." If you can’t calculate AdjBW, you shouldn’t be writing scripts. Period.
Linda Migdal
December 9 2025America’s obesity crisis is a symptom of weak character, not a pharmacological anomaly. If people just ate less and moved more, we wouldn’t need all these fancy dosing formulas. This is just another excuse for personal failure.
Tommy Walton
December 10 2025The real tragedy? We’ve known this since the 80s. But the medical-industrial complex prefers convenience over competence. We’re not treating patients. We’re optimizing for billing codes and EHR checkboxes. 🤡
James Steele
December 12 2025The concept of Adjusted Body Weight is not merely a dosing algorithm-it is an epistemological rupture in clinical medicine. It forces us to confront the Cartesian fallacy of the body as a homogenous fluid matrix. Fat is not inert filler. It is a dynamic endocrine organ with its own pharmacodynamic signature. To ignore this is not negligence-it is ontological arrogance.
Louise Girvan
December 14 2025This is all a cover-up. The government is using obesity to justify mass surveillance through health data. They’re tracking your drug levels to predict your behavior. Next they’ll ban sugar because your vancomycin levels were "subtherapeutic." Wake up.