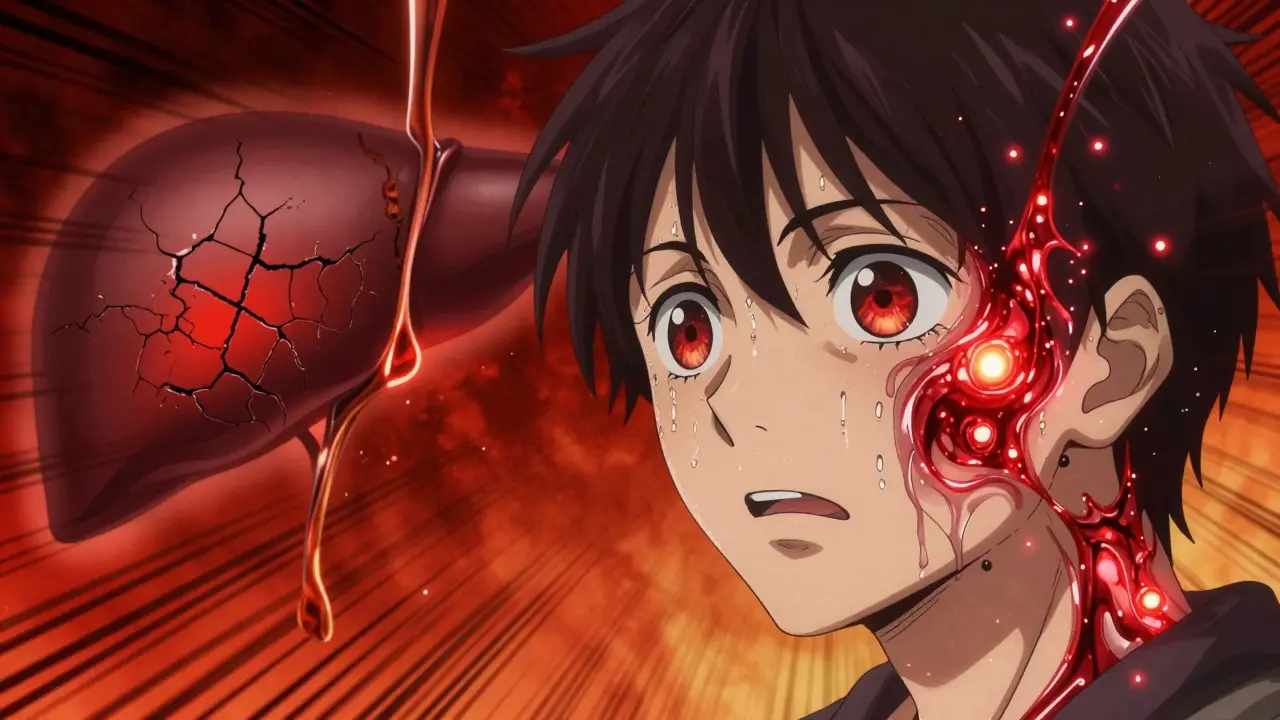
Wilson’s disease isn’t just a rare liver condition-it’s a silent copper overload that can wreck your brain, liver, and kidneys if left unchecked. It starts with a broken gene, ATP7B, that stops your body from getting rid of excess copper. Instead of being flushed out through bile, copper builds up like rust in pipes-first in the liver, then spilling into the bloodstream and settling in the brain and eyes. Left untreated, it’s fatal. But with the right treatment, people with Wilson’s disease can live full, normal lives.
How Copper Goes Wrong in Wilson’s Disease
Your body needs copper. It’s in your enzymes, your nerves, your blood vessels. But too much? That’s poison. In healthy people, the liver uses a protein called ATP7B to pack copper into ceruloplasmin (a transport protein) and dump the rest into bile for elimination. In Wilson’s disease, that protein is broken. Mutations in the ATP7B gene mean copper doesn’t get loaded onto ceruloplasmin, so serum levels drop below 20 mg/dL (normal is 20-50). At the same time, copper doesn’t get excreted into bile. Normal biliary copper output is 1-1.5 mg per day. In Wilson’s, it’s under 0.5 mg.
At first, liver cells try to cope by trapping copper in metallothionein proteins. But once those are full-usually after years of buildup-copper leaks into the blood as free, unbound copper. This is the dangerous kind. It doesn’t stick to proteins. It floats around, seeking out tissues with high metabolic activity: the basal ganglia in the brain, the cornea of the eye, the kidneys. That’s why people with Wilson’s end up with tremors, stiffness, or trouble speaking. And why nearly all neurologically affected patients develop Kayser-Fleischer rings: a rusty-brown halo around the iris, visible only with an eye exam.
Why Diagnosis Is So Hard
Wilson’s disease mimics other conditions. It looks like autoimmune hepatitis. It acts like Parkinson’s. It shows up as unexplained liver enzyme spikes. That’s why the average person waits 2.7 years for a correct diagnosis. Many are misdiagnosed twice-or even three times-before someone checks their 24-hour urinary copper.
Here’s what sets Wilson’s apart:
- Low ceruloplasmin (<20 mg/dL)
- High urinary copper (>100 μg/24h in liver cases, though it drops in neurological cases)
- Kayser-Fleischer rings (present in 95% of those with neurological symptoms)
- High liver copper (>250 μg/g dry weight)
But here’s the catch: kids under 5 often don’t have Kayser-Fleischer rings yet, and their ceruloplasmin can be low for normal reasons. That’s why the 2023 diagnostic guidelines now include genetic testing for ATP7B mutations as a definitive score. If you have two disease-causing mutations, you have Wilson’s-even if other tests are borderline.
Chelation Therapy: The Lifeline
Chelation therapy is the backbone of treatment. It’s not a cure, but it’s a way to force your body to get rid of the copper you can’t excrete on your own. The goal? Pull copper out of your organs and flush it through urine-without making you copper-deficient.
There are three main chelators:
- D-penicillamine (Cuprimine®): The oldest and cheapest option. Dosed at 750-1,500 mg/day for adults. But it causes side effects in half of users: nausea, metallic taste, skin rashes, and, worst of all, neurological worsening in 20-50% during the first few weeks. Some patients get worse before they get better.
- Trientine (Syprine®): A better-tolerated alternative. Less likely to trigger neurological flares. But it costs over $1,850 a month in the U.S.-six times more than penicillamine. It can also cause iron deficiency in up to 35% of users.
- Zinc acetate (Galzin®): Not a chelator, but a blocker. It tells your gut to make metallothionein, which traps dietary copper so it can’t be absorbed. Used for maintenance after initial chelation, or for asymptomatic people. It’s safe, well-tolerated, and costs around $450/month.
Many patients start with penicillamine or trientine, then switch to zinc for long-term control. Zinc alone works for 92% of people if serum free copper stays below 10 μg/dL.

The Treatment Tightrope
Chelation isn’t simple. Too little copper, and you risk anemia, nerve damage, or immune problems. Too much, and your brain keeps getting damaged. Monitoring is non-negotiable.
Here’s what’s required:
- Every 3 months: Liver enzymes (ALT, AST), complete blood count
- Every 3 months: Serum free copper (target: <10 μg/dL)
- Every 6 months: 24-hour urinary copper (target: 200-500 μg/24h during maintenance)
- Annual eye exam for Kayser-Fleischer rings
And diet? You need to limit copper to under 1 mg per day. That means avoiding liver, shellfish, nuts, chocolate, mushrooms, and even some tap water from copper pipes. Most patients struggle with this. One survey found 89% found it hard to stick to.
New Hope on the Horizon
Chelation therapy has been around since the 1950s. But new drugs are coming fast.
In 2023, a new copper-binding polymer called CLN-1357 showed an 82% drop in free serum copper in just 12 weeks-with zero neurological worsening. That’s huge. Traditional chelators often trigger flares. This one didn’t.
Another drug, WTX101 (bis-choline tetrathiomolybdate), got FDA breakthrough therapy designation in early 2023. In trials, it prevented neurological decline in 91% of patients-better than trientine’s 72%. It’s designed to cross the blood-brain barrier more effectively, targeting copper buildup in the brain directly.
And then there’s gene therapy. Early trials using a viral vector to deliver a working ATP7B gene into liver cells are showing safety in six patients. It’s still early, but if it works, it could one day replace lifelong chelation.

What Patients Really Say
On forums like r/WilsonsDisease, stories are raw and real.
One user switched from penicillamine to zinc after severe kidney damage. Within six months, their liver enzymes dropped from 145 to 38. Another, after seven years of misdiagnosis, finally got diagnosed when their 24-hour urine copper hit 380 μg/24h-then suffered a neurological flare from penicillamine. They’re now on zinc and doing better.
Side effects are the biggest reason people miss doses. Nausea. Metallic taste. Fatigue. A third of patients skip pills. But those who stick with it? They live. They work. They raise kids. They travel.
The key isn’t perfection. It’s consistency. Even if you miss a dose, don’t give up. Talk to your doctor. Adjust. Switch meds. There’s always another option.
Why This Matters
Wilson’s disease is rare-1 in 30,000. But it’s not rare enough to ignore. If you have unexplained liver disease, tremors, or psychiatric symptoms before age 35, get tested. Don’t wait for the perfect test. If ceruloplasmin is low and urinary copper is high, treat it like Wilson’s until proven otherwise.
And if you’ve been diagnosed? You’re not alone. With today’s treatments, your life expectancy is normal. Your brain can heal. Your liver can recover. The copper doesn’t have to win.
The real challenge isn’t the science. It’s awareness. It’s access. In low-income countries, diagnosis delays can hit five years. In the U.S., cost keeps some from getting the best drugs. But progress is real. The tools are here. The knowledge is here. Now we just need to use them.
Can Wilson’s disease be cured?
No, Wilson’s disease cannot be cured yet, but it can be effectively managed for life. With consistent chelation therapy or zinc maintenance, copper levels stay under control, organ damage stops progressing, and most people live normal lifespans. Gene therapy is in early trials and may one day offer a true cure.
How do I know if I have Wilson’s disease?
If you’re under 35 and have unexplained liver problems, neurological symptoms like tremors or stiffness, or psychiatric changes, ask for testing. Key tests include serum ceruloplasmin, 24-hour urinary copper, serum free copper, and a slit-lamp eye exam for Kayser-Fleischer rings. Genetic testing for ATP7B mutations is now considered definitive.
Why does D-penicillamine make symptoms worse?
D-penicillamine pulls copper out of tissues too quickly, releasing free copper into the bloodstream. This can flood the brain with copper before the body can clear it, worsening neurological symptoms. That’s why many doctors start with zinc or switch to trientine if neurological symptoms are present.
Can I take vitamin supplements with Wilson’s disease?
Avoid supplements with copper unless prescribed. Most multivitamins contain 2 mg of copper-double your daily limit. Zinc supplements are safe and often recommended, especially with chelation therapy. Iron may be needed if you’re on trientine, as it can cause deficiency. Always check with your doctor before starting any supplement.
Is Wilson’s disease hereditary?
Yes. Wilson’s disease is autosomal recessive, meaning you inherit two faulty copies of the ATP7B gene-one from each parent. If both parents are carriers (1 in 90 people), each child has a 25% chance of having the disease. Siblings of diagnosed patients should be tested, even if they show no symptoms.
What happens if I stop my medication?
Stopping treatment leads to rapid copper reaccumulation. Liver damage can return within months. Neurological symptoms can worsen permanently. Even if you feel fine, stopping meds is dangerous. Wilson’s disease requires lifelong therapy. Missing doses increases your risk of irreversible damage.


Jane Wei
December 17 2025Wow, I had no idea copper could be this dangerous. My uncle had weird tremors for years and no one could figure it out until they tested for Wilson’s. He’s been on zinc for 8 years now and barely needs anything else. Life-changing stuff.
Also, that Kayser-Fleischer ring thing? Wild that it’s literally visible if you know where to look. Eye exam = free diagnostic tool.
Erik J
December 18 2025Interesting how the ATP7B mutation affects ceruloplasmin loading. I wonder if there’s any research on partial function alleles-like, do people with one working copy ever show mild symptoms? Or is it strictly recessive?
Martin Spedding
December 19 2025penicillamine is a nightmare. my cousin went from ‘just tired’ to ‘can’t hold a spoon’ in 3 weeks on it. trientine’s expensive but worth it if you can afford it. zinc is the real MVP for maintenance.
Virginia Seitz
December 20 2025I have a friend with this 😢 so glad there’s treatment! 🙏
Brooks Beveridge
December 21 2025It’s wild how medicine often treats symptoms before it sees the root. Wilson’s is a perfect example-people get labeled as ‘Parkinson’s’ or ‘autoimmune’ for years while the real problem just keeps building up. The fact that we now have genetic testing as a definitive tool? That’s progress. Not just science-human dignity.
Sachin Bhorde
December 21 2025yo the 24hr urinary copper is the golden ticket, but most docs dont even think of it unless u r a med student or have a fam hx. also, zinc is underrated-its like a copper sponge in the gut. no flares, no side effects, just chill. but if u r in india, good luck getting trientine without begging your doctor 12 times. we got penicillamine or nothing.
Joe Bartlett
December 23 2025Yup, we got this sorted in the NHS. Penicillamine’s free, zinc’s cheap. Americans pay $2k for a pill? Madness. You’d think a genetic disease would be a priority, not a profit center.
Marie Mee
December 24 2025what if this is all a big pharma lie to sell chelators? what if copper is actually good and they’re poisoning us with zinc? i read a blog that said the liver was meant to store copper and the whole thing is a scam. my cousin died and they said it was Wilson’s but i think they just gave her too much penicillamine.
Salome Perez
December 24 2025While the clinical management of Wilson’s disease has evolved significantly, particularly with the integration of molecular diagnostics, it remains imperative to emphasize the multidisciplinary approach required for optimal outcomes. Hepatologists, neurologists, genetic counselors, and nutritionists must collaborate to ensure that chelation protocols are tailored to individual phenotypes, while monitoring for both copper toxicity and iatrogenic micronutrient deficiencies. The advent of affordable genetic sequencing has fundamentally altered diagnostic paradigms, yet access disparities persist globally.
Evelyn Vélez Mejía
December 25 2025The real tragedy isn’t the disease-it’s the years lost to misdiagnosis. Every patient who endures a two-year diagnostic odyssey is a testament to systemic fragmentation in medicine. We treat organs in silos: liver specialists see ALT elevations, neurologists see tremors, psychiatrists see ‘psychogenic movement disorder.’ But Wilson’s doesn’t care about departmental boundaries. It’s a systemic failure of the ATP7B protein-and until our healthcare system learns to see patients as integrated systems, not isolated symptoms, we’ll keep failing them. Genetic screening should be routine in unexplained liver or movement disorders, period.