Most people think of a rotator cuff tear as something that happens to athletes or weightlifters. But the truth? Rotator cuff tears are far more common than you think - especially after 40. In fact, over half of people over 60 have a tear in their shoulder without even knowing it. No pain. No symptoms. Just a worn-out tendon. So if you’re dealing with shoulder pain, stiffness, or weakness when lifting your arm, it’s not just "getting older." It could be a rotator cuff tear - and knowing how to diagnose and treat it properly makes all the difference.
How Doctors Spot a Rotator Cuff Tear
Before any scan, your doctor will start with your hands. That’s right - physical exams still come first. They’ll move your arm in specific ways to test for pain and weakness. Tests like the Empty Can, Neer impingement, and Hawkins-Kennedy aren’t just random moves. They’re proven ways to find which tendon is damaged. If you feel sharp pain when your arm is lifted overhead, or if you can’t hold your arm out to the side without it dropping, those are red flags.
But here’s the catch: physical exams alone can’t tell you the size or depth of the tear. That’s where imaging comes in. The first imaging test? X-ray. It doesn’t show tendons, but it shows bone. Are there bone spurs? Is the joint arthritic? Is the shoulder aligned right? These details change how you treat the tear. Over 90% of patients get an X-ray before anything else.
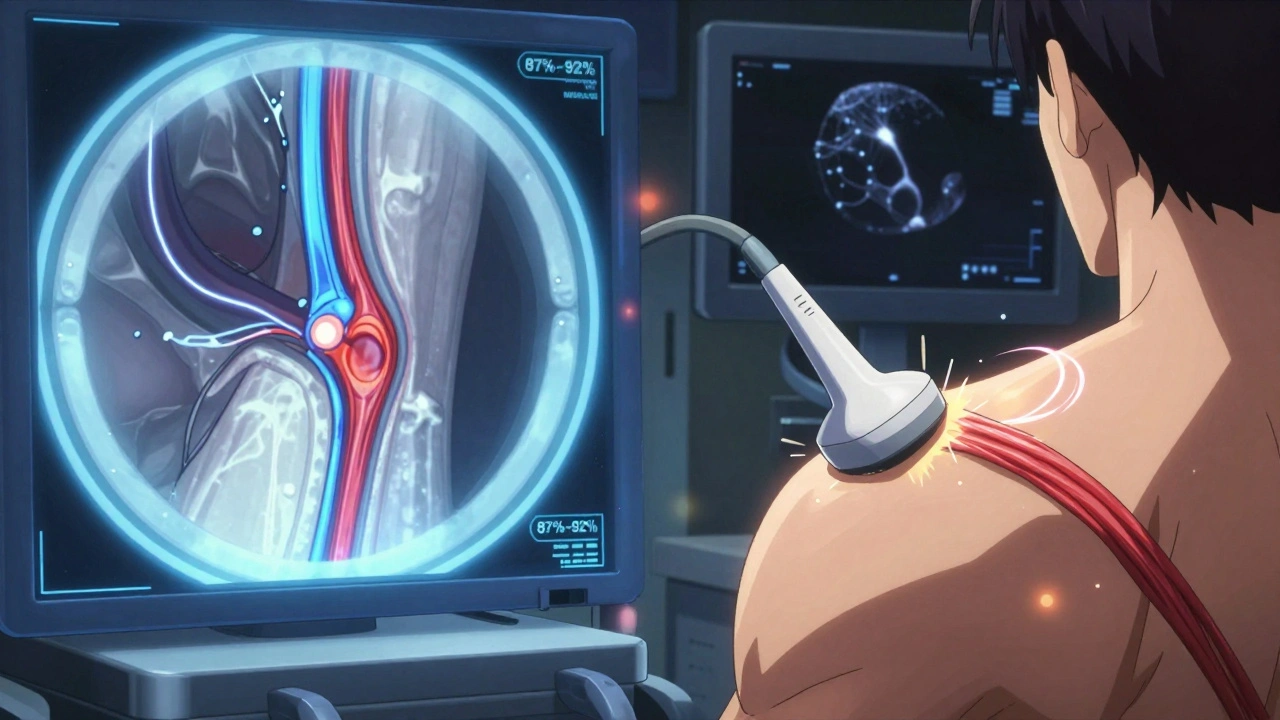
Now, for the actual tear - that’s where MRI and ultrasound come in. Both can see soft tissue. MRI gives you a detailed, high-res picture of the whole shoulder. It shows if the tear is partial or full-thickness, how big it is, and even if the muscle has started to waste away. MRI is accurate about 92% of the time for full-thickness tears. But it’s expensive - often $500 to $1,200 - and you can’t use it if you have metal implants like pacemakers or joint replacements.
Ultrasound is the quiet alternative. It’s cheaper - around $200 to $400 - and you can watch the tendon move in real time. If you lift your arm and the tendon snaps or doesn’t glide smoothly, the ultrasound catches it. Studies show it’s 87% to 91% accurate for full-thickness tears. Patients prefer it too. In one survey, 92% chose ultrasound over MRI because it’s faster, quieter, and doesn’t feel like being locked in a tube.
But ultrasound has a downside: it’s only as good as the person holding the probe. Only 45% of general radiologists are trained to read shoulder ultrasounds well. If your clinic doesn’t have a specialist, you might miss a small tear. That’s why MRI is still the gold standard for surgical planning. If your doctor thinks you need an operation, they’ll likely order an MRI to map out the damage before cutting.
Rehab: Can You Fix It Without Surgery?
Here’s the good news: most people don’t need surgery. About 85% of those with partial-thickness tears get better with rehab alone. Even some full-thickness tears - especially in older or less active people - can be managed without an operation.
Rehab isn’t just doing stretches. It’s a step-by-step process that takes months. Phase one (weeks 1-6) is all about protecting the shoulder. No lifting. No reaching. Just passive movement - someone else moves your arm for you to keep the joint loose. This prevents stiffness without stressing the tear.
Phase two (weeks 6-12) adds active-assisted motion. You start using your own muscles, but with help - resistance bands, pulleys, or even your other arm. The goal? Regain full range of motion without pain.
Phase three (after week 12) is strengthening. This is where you rebuild the rotator cuff muscles: supraspinatus, infraspinatus, teres minor, subscapularis. Exercises like external rotation with a band, scapular squeezes, and wall push-ups are key. It’s slow. It’s boring. But skipping this phase is why some people get worse after rehab.
Studies show that people who stick with rehab for at least 3 months have a 70% higher chance of avoiding surgery. And if you’re over 65, your odds of success without surgery are even better. The American Academy of Orthopaedic Surgeons now recommends trying 6 to 8 weeks of physical therapy before ordering an MRI - because many tears are just part of aging, not emergencies.
Surgery: When and How It’s Done
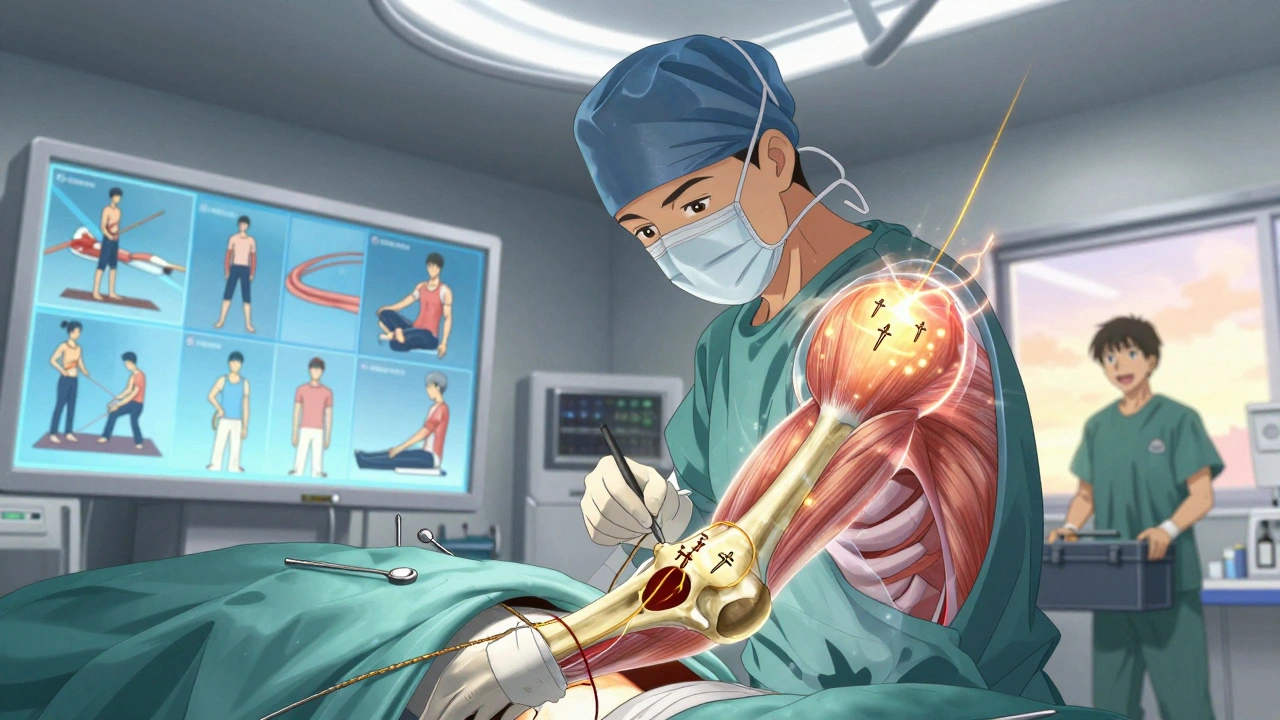
Surgery isn’t a last resort - it’s a smart choice for the right person. If you’re under 65, active, and have a full-thickness tear that’s causing real weakness or pain, surgery often gives the best long-term result. The type of surgery? Almost always arthroscopic. In 90% of cases today, surgeons use small cameras and tiny instruments to repair the tendon through 3-4 half-inch incisions.
Arthroscopic repair has replaced open surgery because it’s less invasive. Recovery is faster. Infections are rarer. Complication rates are about 30% lower than with open surgery. And you’re back to daily tasks like dressing or driving sooner - often within 4 to 6 months instead of 8 to 12.
During the procedure, the surgeon cleans up frayed edges, removes bone spurs that were rubbing on the tendon, and reattaches the torn tendon to the bone using small anchors. These anchors hold the tendon in place while it heals - like stitches in a torn shirt, but buried in bone.
For massive tears - over 3 centimeters - things get trickier. The tendon may be too short or too weak to reattach. That’s when surgeons might use a patch graft or try to transfer another tendon. These are complex cases, and success rates drop. About 27% of large tears retear after surgery, compared to just 12% for small ones.
There’s also talk about PRP (platelet-rich plasma) injections during surgery to speed healing. But the evidence is shaky. The Cochrane Review found only moderate benefit - not enough to make it standard. Same with stem cell injections. They’re trendy, but not proven.
What Happens After Surgery?
Post-op rehab is just as important as the surgery itself. Gone are the days of wearing a sling for 6 weeks. Today, most patients start gentle passive motion the day after surgery. Why? Early movement prevents scar tissue from locking the joint. But you still can’t lift, push, or pull for 3 months.
Weeks 1-6: Passive motion only. Physical therapist moves your arm. You do pendulum swings and gentle stretches.
Weeks 6-12: Active motion begins. You start moving your arm on your own, with light resistance.
Weeks 12-24: Strengthening. Band exercises, light weights, scapular control. No overhead lifting until 4-6 months.
Full recovery? Most people feel 80% better by 6 months. But the tendon takes a full year to fully heal. That’s why you can’t rush back to tennis, lifting, or manual labor too soon. Retear risk is highest between 3 and 6 months - right when people start feeling good and think they’re done.
Long-Term Outcomes: What to Expect
Five years after surgery, 82% of patients say they’re happy with the result. Pain is down. Strength is up. Sleep is better. But not everyone gets back to full function. Retears happen. Muscle atrophy can set in. And if you had a big tear to begin with, you might never regain 100% strength.
That’s why prevention matters. Keep your rotator cuff strong. Do regular shoulder stability exercises. Avoid repetitive overhead motions if you’re over 50. If you feel a dull ache after gardening or painting, rest it. Don’t push through pain.
And if you’re told you need surgery - get a second opinion. Ask if rehab has been tried. Ask what size the tear is. Ask if your muscle quality looks good on the MRI. Those details change everything.
What’s Next in Rotator Cuff Care?
The field is changing fast. AI is starting to help read MRIs. A 2023 study showed deep learning algorithms could tell partial from full-thickness tears with 89% accuracy - faster and more consistent than some radiologists. That could mean quicker diagnoses and fewer missed tears.
Ultrasound is also getting smarter. New handheld devices are now used by orthopedic surgeons in clinics, not just radiologists. You walk in, get scanned right away, and get results before you leave the room.
One thing won’t change: the importance of matching treatment to the person. A 70-year-old gardener with a small tear doesn’t need the same treatment as a 45-year-old carpenter with a large tear. The goal isn’t just to fix the tendon - it’s to get you back to your life.



Chase Brittingham
December 4 2025Just had my third shoulder MRI last month after years of dull aches. Turned out to be a partial tear. I was ready to quit lifting entirely, but my PT said 80% of people like me improve with rehab. Three months in, I can finally reach for the top shelf again. No surgery needed. Seriously, don’t panic if you get diagnosed-give rehab a real shot.
Rebecca Braatz
December 5 2025If you're over 50 and your shoulder hurts after painting or gardening, stop blaming age. It’s not ‘just wear and tear’-it’s your rotator cuff screaming for attention. Start with band work. Do 3 sets of external rotations every other day. No weights. Just control. Your future self will thank you.
Rachel Bonaparte
December 5 2025Let’s be real-big pharma and ortho corporations want you to believe surgery is the only answer. But the truth? They profit from MRIs, implants, and rehab packages. Ultrasound is cheaper, faster, and just as accurate-if you can find a skilled tech. Most clinics don’t even have one. That’s not an accident. It’s business. And if you’re over 60? Your body’s been healing itself for decades. Why let a surgeon mess with it now?
Also, PRP? Stem cells? Please. These are just fancy placebos wrapped in marketing. I’ve seen patients pay $5k for injections that did nothing. Meanwhile, the real fix-consistent, patient rehab-is ignored because it doesn’t come with a price tag.
Scott van Haastrecht
December 5 2025Here’s the real issue: 90% of people who get diagnosed with a rotator cuff tear don’t have symptoms. That means half the MRIs being ordered are unnecessary. And the other 10%? They’re the ones who ignored the pain for years and now have muscle atrophy. You think surgery fixes that? Nope. It just delays the inevitable. This isn’t medicine-it’s damage control for people who refused to move correctly for 20 years.
And don’t get me started on ‘passive motion’ rehab. If your shoulder’s weak, you don’t need someone else moving it. You need to rebuild strength from the ground up. Passive movement is for people who want to feel like they’re doing something without actually doing anything.
Isabelle Bujold
December 6 2025I’m a physiotherapist in Toronto and I see this every week. People come in terrified after an MRI shows a ‘full-thickness tear.’ They’re convinced they need surgery. But when we go through their history-no trauma, no sudden injury, just gradual stiffness and weakness-it’s almost always a degenerative tear, not a traumatic one. And guess what? Most respond beautifully to rehab.
Phase one is non-negotiable: protect the tendon. No lifting, no reaching, no pushing. Sounds extreme, but if you skip this, you’re just re-injuring it. I had a 72-year-old client who couldn’t lift a coffee cup. Six weeks of passive motion, then gradual active work. By month four, she was gardening again. No surgery. Just patience.
The problem is, everyone wants a quick fix. But the rotator cuff doesn’t heal like a sprained ankle. It’s a slow, boring, frustrating process. And that’s why so many people quit at week 8 and blame the treatment. It’s not the rehab-it’s the mindset.
Also, ultrasound is underused. I’ve got a portable machine in my clinic. We scan on the spot. If the tendon glides, it’s fine. If it snaps or doesn’t move, we know. No waiting weeks for an MRI. And it’s way less stressful for the patient. But insurance? They’d rather pay for an MRI. It’s easier to code.
And yes, surgeon training matters. I’ve seen cases where a radiologist missed a small tear because they weren’t trained in shoulder US. That’s not the tech’s fault-it’s the system. If your doctor orders an MRI without checking your movement first, find a new one.
One last thing: muscle quality. If the MRI shows fatty infiltration in the supraspinatus, surgery isn’t going to fix that. The muscle’s already gone. Rehab won’t bring it back, but it can help the other muscles compensate. That’s still a win. Don’t let a scan define your potential.
And for those asking about PRP or stem cells? The evidence is weak. I’ve seen patients spend $3k on injections that did nothing. Meanwhile, the person next to them who did 12 weeks of scapular control and external rotation with bands? Back to hiking. The difference isn’t the tech-it’s the discipline.
So if you’re reading this and you’ve been told you need surgery-ask for a rehab trial. Six to eight weeks. No pressure. No rush. Just movement. You might be surprised.
Bill Wolfe
December 7 2025Wow. Just wow. 🤦♂️ So let me get this straight-you’re telling people over 60 with a tear to just ‘do stretches’? 😂 You’re not a doctor, are you? Or maybe you’re just one of those ‘natural healing’ cranks who thinks bones grow back with crystals and affirmations. 🙄
Let me break it down for you: if your tendon is torn, it’s TORN. No amount of band work will glue it back together. And if you’re telling someone to wait 6 months for rehab to ‘work’ while they’re in constant pain? That’s not wisdom-that’s negligence. Surgery isn’t a last resort. It’s the only thing that fixes a structural failure.
And don’t even get me started on ultrasound. You think a tech with a handheld probe can match an MRI’s resolution? Please. You’re risking permanent damage because you’re too cheap to pay for the real diagnostic tool. 🤡
And PRP? Stem cells? You think I don’t know these are cash grabs? Of course I do. But at least they’re *trying* something. Rehab for 6 months? That’s just letting the body rot while you wait for it to magically heal. 🤷♂️
If you’re active, under 65, and have a full-thickness tear? Surgery. Period. No debate. No ‘maybe.’ No ‘try rehab first.’ You’re not a 70-year-old gardener-you’re a human being with a functional body that deserves to work. Stop being so passive.
Ollie Newland
December 8 2025Interesting breakdown. One thing I’d add is the role of scapular dyskinesis in rotator cuff pathology. Often, the tear isn’t the primary issue-it’s the faulty kinematics upstream. If the scapula isn’t stabilizing properly, you’re overloading the cuff regardless of tendon integrity. That’s why rehab needs to start with scapular retraining before even touching rotator cuff exercises.
Studies show that 68% of patients with chronic shoulder pain have altered scapular motion patterns. If you skip that, you’re treating the symptom, not the cause. External rotation bands are great, but if your shoulder blade is winging, you’re just putting more strain on an already compromised system.
Also, the term ‘full-thickness tear’ is misleading. It’s not binary. There’s a spectrum: partial-thickness intratendinous, articular-sided, bursal-sided, and then full-thickness. Location matters. Articular-sided tears respond better to rehab. Bursal-sided? Often more symptomatic. MRI helps, but clinical correlation is king.
And yes-ultrasound is undervalued. But it’s not just about the operator. The machine matters too. High-frequency linear probes (12-18 MHz) are essential. Most clinics still use low-end machines designed for abdominal scans. No wonder they miss small tears.
Lastly, the 85% rehab success rate? That’s for *partial* tears. Full-thickness? More like 50-60% without surgery. And if you’re over 65 with low functional demands? Sure, conservative management makes sense. But if you’re a carpenter, a swimmer, or even a gardener who lifts bags of soil? Don’t gamble.
Michael Feldstein
December 9 2025My dad had a tear at 68. Didn’t want surgery. Did rehab for 5 months. Now he’s back to fixing his bike, hanging Christmas lights, even carrying groceries. No pain. No meds. Just consistency.
He didn’t do fancy stuff. Just daily pendulum swings, wall climbs, and band rotations. Three times a day. No days off. That’s it.
People think rehab is about intensity. It’s not. It’s about repetition. And patience.
jagdish kumar
December 10 2025Tears are nature’s way of saying: stop forcing what’s already worn out.
Benjamin Sedler
December 12 2025Okay, but what if the real problem isn’t the tear-it’s the fact that we’ve been taught to lift with our shoulders instead of our hips? What if the rotator cuff is just the collateral damage of decades of bad form, CrossFit bros, and yoga influencers telling people to ‘reach for the sky’ when their scapulae are stuck in a permanent slump?
Maybe we’re not treating the tear… we’re treating the symptom of a culture that turned movement into performance.
Also, why is MRI the ‘gold standard’? Because it’s expensive and profitable. Not because it’s better. The body doesn’t care about pixels. It cares about function. And function? That’s measured by how high you can reach, not how bright the tear looks on a screen.
Jessica Baydowicz
December 12 2025You’re not broken. You’re just out of practice. Your shoulder didn’t fail you-it’s been waiting for you to listen.
Start today. Not tomorrow. Not after your MRI. Right now. Do 5 minutes of pendulum swings. Then 5 minutes of scapular squeezes. Then 5 minutes of external rotation with a band.
That’s it. No equipment. No cost. Just you and your body.
Progress isn’t linear. Some days you’ll feel better. Some days worse. That’s normal. But if you show up? You’ll win.
I’ve seen it a hundred times. People think they need surgery because they’re scared. But the real surgery? It’s showing up every day when you don’t feel like it.
val kendra
December 13 2025Rehab works if you do it right. Not just stretches. Strength. Control. Consistency. I did 12 weeks. No pain now. No surgery. Just dumbbells and patience.
George Graham
December 14 2025I’m a former physical therapist from Ohio. Used to work with older patients who came in with ‘rotator cuff tear’ on their chart and panic in their eyes. What I learned? Most of them didn’t need surgery. They needed someone to sit with them. To explain that pain doesn’t equal damage. That healing isn’t fast. That their body wasn’t broken-it was just tired.
One woman, 74, couldn’t lift her arm past 30 degrees. We started with passive motion, then gentle pendulums. By week 10, she was brushing her hair again. She cried. Not because she was healed-but because she felt heard.
Sometimes the best treatment isn’t the scan or the surgery. It’s the person who says: ‘I believe you can do this.’
John Filby
December 16 2025Just had my first ultrasound for shoulder pain. The tech showed me the tendon moving in real time. Saw the little gap where it was torn. Didn’t feel scary-kinda fascinating. My doctor said I’m a candidate for rehab. No MRI yet. Just started the band exercises. Feeling hopeful.