Why Lung Cancer Screening Matters More Than Ever
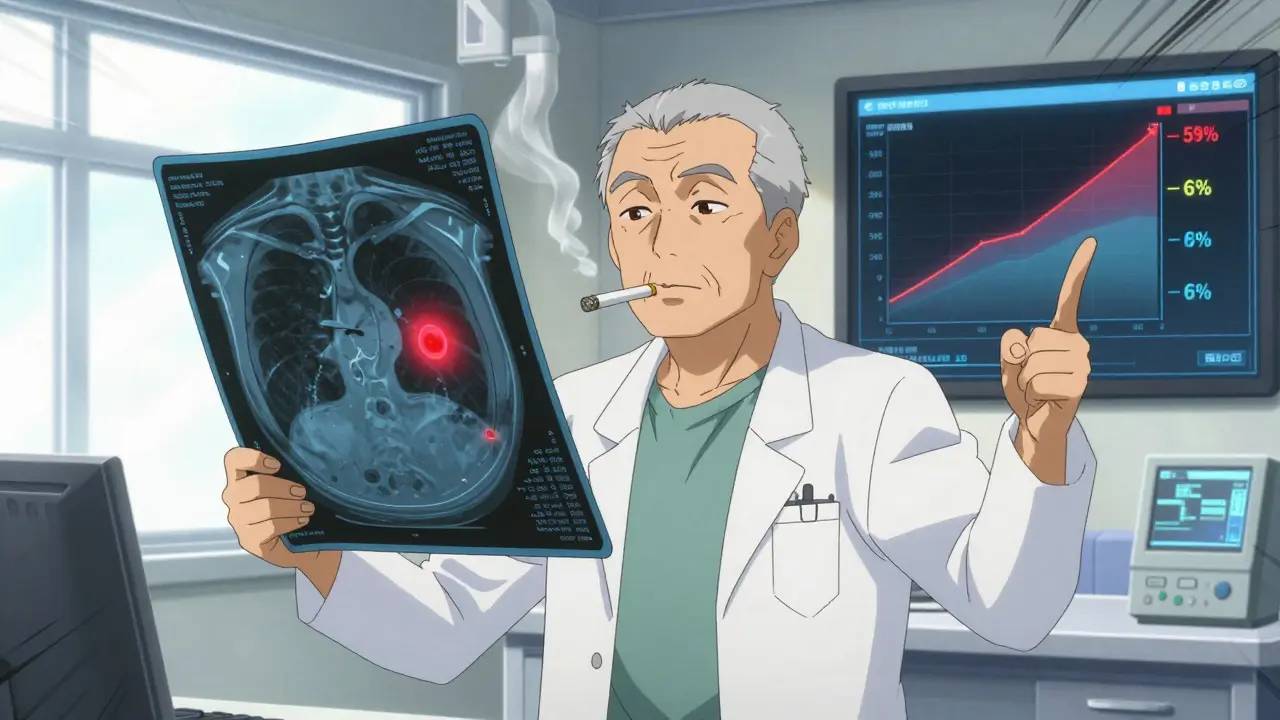
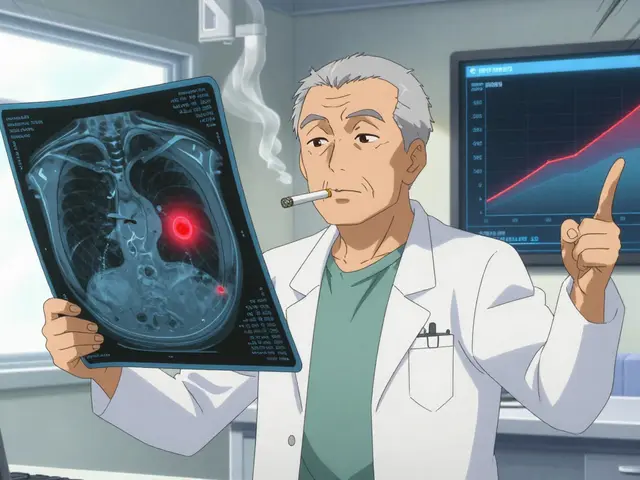
If you’ve smoked for 20 years or more, even if you quit years ago, your risk of lung cancer hasn’t disappeared. In fact, it’s still higher than someone who never smoked. That’s why screening isn’t just a good idea-it’s a life-saving step. The truth is, most lung cancers are found too late. Only about 23% of cases are caught early, when treatment has the best chance. But when lung cancer is found early with a low-dose CT scan, the five-year survival rate jumps from 6% to 59%. That’s not a small improvement. That’s the difference between dying and living.
Who Should Get Screened? The New Rules
The guidelines changed in 2023, and they’re now much more inclusive. The American Cancer Society says anyone aged 50 to 80 with a 20-pack-year smoking history should get screened annually-no matter how long ago they quit. A pack-year means smoking one pack a day for a year. So 20 pack-years could be one pack a day for 20 years, two packs a day for 10 years, or even half a pack a day for 40 years. That’s it. No cutoff at 15 years after quitting anymore.
Before, many people were left out. If you quit smoking 18 years ago, you were no longer eligible under older rules. But research shows your risk stays high for decades. A 2022 JAMA Oncology study found former smokers 15 to 30 years after quitting still had 2.5 times the risk of lung cancer compared to never-smokers. The old rule wasn’t just outdated-it was dangerous.
How Screening Works: The Low-Dose CT Scan
The test is simple. You lie on a table, take a breath, and hold it for about 10 seconds. No needles, no fasting, no prep. The machine uses 70-80% less radiation than a regular CT scan. That’s why it’s called low-dose CT, or LDCT. It’s designed to find tiny nodules in the lungs before they grow into tumors. The scan itself takes less than a minute.
But here’s the catch: most positive results aren’t cancer. The National Lung Screening Trial found that 96.4% of people with a positive scan didn’t have cancer. That means a lot of follow-up tests, biopsies, and anxiety. That’s why screening is only recommended for people who are healthy enough to handle treatment if cancer is found. If you have heart failure, severe COPD, or other conditions that limit life expectancy, screening won’t help you-and might hurt you with unnecessary procedures.

Why So Few People Are Getting Screened
Despite the clear benefits, only about 5.7% of eligible people in the U.S. are actually getting screened. That’s not a technical problem. It’s a system failure. Most primary care doctors still don’t know the updated guidelines. A 2022 AMA survey showed 42% of them weren’t aware of the 2021 USPSTF changes. Patients don’t know they qualify. And even when they do, there aren’t enough accredited centers.
In rural areas, there are 67% fewer screening facilities than in cities. Medicare covers the scan for people 50 to 77 with a 20-pack-year history who smoke or quit within the last 15 years. But some private insurers still require 30 pack-years and only cover people 55 and older. That creates confusion and delays. And without a structured process-risk assessment, shared decision-making, follow-up tracking-screening just doesn’t stick.
How to Make Screening Work: What Actually Helps
Programs that work use three key tools: electronic reminders, patient navigators, and quit-smoking support. A 2021 JAMA Internal Medicine study showed that when EHR systems automatically flagged eligible patients, screening rates jumped by 32%. Patient navigators-who help schedule appointments, explain results, and answer questions-boost adherence by 27%. And here’s something surprising: 70% of current smokers who get screened say they want to quit. But only 30% are offered help. That’s a missed opportunity. Screening isn’t just about finding cancer. It’s a chance to stop smoking before it’s too late.
Targeted Therapy: When Early Detection Meets Precision Medicine
Screening finds cancer early. But what you do next matters just as much. For early-stage lung cancer, surgery is often the first step. But now, doctors can add targeted therapy after surgery to stop the cancer from coming back. The drug osimertinib, approved in 2020, is a game-changer. In the ADAURA trial, it cut the risk of recurrence or death by 83% in patients with EGFR mutations. That’s not a small benefit. That’s almost turning early-stage lung cancer into a chronic, manageable condition.
Here’s the kicker: by 2025, experts expect 70% of early-stage lung cancers found through screening will have these actionable mutations. But only 30% of late-stage cancers do. That’s why screening isn’t just about catching cancer early-it’s about catching the right kind of cancer early. The more you catch early, the more you can treat with these precision drugs.
What’s Coming Next: AI and Liquid Biopsies
Artificial intelligence is already helping. The FDA approved LungQ by Riverain Technologies in January 2023. This software analyzes CT scans and flags nodules with more accuracy. In trials, it reduced unnecessary follow-ups by 22%. That means fewer scans, less stress, and lower costs.
Even more exciting are liquid biopsies-blood tests that look for cancer DNA floating in the bloodstream. Right now, these tests can’t replace CT scans. But they’re getting closer. Multiple clinical trials are testing whether a blood test can detect lung cancer signals before a tumor shows up on a scan. If this works, screening could become even earlier, even more precise. Imagine a simple blood test every year, followed by a CT scan only if needed. That’s the future.
What You Need to Do Right Now
If you’re between 50 and 80 and have smoked at least 20 pack-years-whether you still smoke or quit 20 years ago-ask your doctor about screening. Don’t wait for them to bring it up. Bring it up yourself. Say: “I’m eligible for lung cancer screening. Can you order a low-dose CT scan?”
If you’re still smoking, this is your moment. Screening gives you a reason to quit. And if you’re ready to quit, ask for help. Programs that combine screening with counseling and medication are the most effective. Quitting now cuts your lung cancer risk by half within five years.
What’s Not Covered
Screening doesn’t replace quitting. It doesn’t guarantee you won’t get cancer. And it won’t help if you’re too sick to treat cancer if it’s found. If you’re under 50, or your smoking history is less than 20 pack-years, screening isn’t recommended. If you have symptoms-coughing up blood, chest pain, weight loss-you need diagnostic tests, not screening.
Do I need a referral to get screened for lung cancer?
Yes, you usually need a referral from your doctor. Screening isn’t something you can just walk in for. Your provider must first confirm you meet the criteria and have a shared decision-making visit. This is a conversation, not a formality. It should cover your risks, the benefits of screening, and the chance of false positives.
Is lung cancer screening covered by insurance?
Under the Affordable Care Act, most private insurers and Medicare must cover annual low-dose CT screening for eligible people without a copay. Medicare covers people aged 50 to 77 with a 20-pack-year history who currently smoke or quit within the past 15 years. But some commercial insurers still use outdated rules. Always check with your plan. If you’re denied, ask for a written explanation and appeal.
What if my scan shows a nodule?
Most nodules aren’t cancer. But they need monitoring. Your doctor will compare the scan to past ones (if you have them) and may schedule a follow-up CT in 3, 6, or 12 months. If the nodule grows or looks suspicious, you’ll be referred to a specialist. Never ignore a follow-up recommendation. Early action saves lives.
Can non-smokers get screened for lung cancer?
Currently, no major guidelines recommend screening for non-smokers. But about 20% of lung cancer deaths occur in people who never smoked. Research is underway to find better ways to identify high-risk non-smokers-through genetics, air pollution exposure, or family history. For now, if you’re a non-smoker with symptoms, talk to your doctor about diagnostic testing.
How often should I get screened?
Once a year, as long as you’re still eligible and in good health. Skipping a year reduces the benefit. Annual scans are the only proven way to catch cancer early enough to treat it effectively. Don’t wait until you feel sick. By then, it’s often too late.

Edith Brederode
January 20 2026I got my LDCT last year after my cousin died of lung cancer at 58. They found a tiny nodule-turned out to be nothing. But honestly? I cried after the scan. Not from fear. From relief. 😭 I’m 54, quit 12 years ago. If I hadn’t pushed my doctor? I wouldn’t be here typing this.
Screening isn’t scary. Not getting it is.
clifford hoang
January 21 2026Lol. So now we’re all supposed to trust Big Pharma + the government’s new screening agenda? 😏 Who really benefits? The radiology centers. The drug companies pushing osimertinib at $15K/month. The insurance bots who don’t want to pay for 30 pack-year folks.
And don’t get me started on ‘AI analysis’-that’s just a fancy way to say ‘we’re automating misdiagnoses.’ 96% false positives? That’s not medicine. That’s a scam wrapped in a CT scan. 🤖💀
Arlene Mathison
January 21 2026I’m 57, smoked for 22 years, quit 8 years ago. My doctor never mentioned screening until I brought it up. I had to Google it myself.
That scan saved my life. Not because I had cancer-but because it made me realize I still had time to heal. I started walking every morning. Got a therapist. Started cooking real food.
Screening isn’t just about detecting tumors. It’s about waking people up. And if you’re reading this? You’re one step away from your second chance. Do it. 💪❤️
Emily Leigh
January 22 2026Ugh. Another ‘you’re not doing enough’ guilt trip. I quit smoking 10 years ago. I’ve been healthy since. Why do I need a scan? Because some algorithm says so?
And what about all the people who get biopsied for nothing? Anxiety isn’t a side effect-it’s the main product here. 😒
Carolyn Rose Meszaros
January 22 2026My mom got screened last year. Nodule. Follow-up. Another nodule. Then… nothing. No cancer. But she said the whole process made her feel seen. Like someone finally cared enough to look. 🫂
And honestly? The tech is wild. They showed her the scan on a tablet. The AI highlighted the nodule like it was a highlighter mark. Felt like sci-fi. But in a good way. 🤖❤️
Greg Robertson
January 23 2026I work in a rural clinic. We’ve got one CT machine. It’s booked solid. Patients wait 6-8 weeks. Some just give up.
And the insurance denials? Ugh. One guy had 20 pack-years, quit 14 years ago. Insurer said ‘not eligible.’ We had to appeal. Took 3 months. He got the scan. No cancer. But he cried when he got the letter. Said he thought he was a goner.
Screening isn’t perfect. But it’s the best shot we’ve got.
Renee Stringer
January 23 2026I don’t understand why we’re normalizing this. We’re turning a medical intervention into a moral obligation. ‘You smoked? Then you owe us a scan.’
What about people who never smoked but got cancer from radon? Or air pollution? Or genetics? Why are we singling out smokers? It’s not fair. And it’s not medicine-it’s blame.
Courtney Carra
January 25 2026There’s a deeper question here: what does it mean to be ‘eligible’ for life?
Is survival a reward for compliance? A privilege for those who followed the rules? We screen people who smoked 20 pack-years-but what about the ones who worked in asbestos factories? Or lived near coal plants?
Screening feels like a Band-Aid on a bullet wound. We fixate on the symptom, not the system.
And yet… I still got mine. Because I’m scared. And maybe that’s the real tragedy.
thomas wall
January 27 2026The notion that screening is a panacea is not only misleading-it is dangerously reductive. One cannot mitigate the consequences of decades of toxic habit with a single imaging procedure. The real failure lies in public health policy that permits the proliferation of nicotine addiction, then offers a scan as absolution.
One does not cure a moral failure with a machine. One must confront the culture that enables it. And yet, here we are, applauding a CT scan as if it were a moral victory. How profoundly sad.
Manoj Kumar Billigunta
January 27 2026I’m from India. We don’t have this kind of screening. My uncle had lung cancer. He never smoked. Worked in a textile factory. Got diagnosed at stage 4. No CT. No osimertinib. Just pain pills.
When I saw this post, I cried. Not because I’m scared. Because I wish this was normal everywhere. Not just for people who ‘qualified’.
Screening isn’t a privilege. It’s a right. And if you’re reading this and you’re eligible? Do it. For everyone who can’t.
Thomas Varner
January 27 2026I got my scan last month. Nodule. Follow-up in 6 months.
Meanwhile, I started vaping. Just to ‘see if it’s better’.
Yeah, I know. I’m an idiot. But the scan didn’t scare me straight. It just made me feel like I was being watched.
So… I’m still here. Still smoking. Still waiting.
Maybe next year.