Every year, millions of people reach for an OTC pain reliever or allergy pill without thinking twice. But just because you can buy these meds off the shelf doesn’t mean they’re harmless. NSAIDs, acetaminophen, and antihistamines are the most common over-the-counter drugs in the UK and US - and each carries hidden risks if used wrong.
What You’re Really Taking: NSAIDs, Acetaminophen, and Antihistamines
NSAIDs like ibuprofen (Advil, Motrin) and naproxen (Aleve) work by blocking enzymes that cause inflammation, pain, and fever. They’re great for sprains, arthritis, or menstrual cramps. But they don’t just target the bad stuff - they also suppress protective stomach lining, which is why regular use can lead to ulcers or internal bleeding.
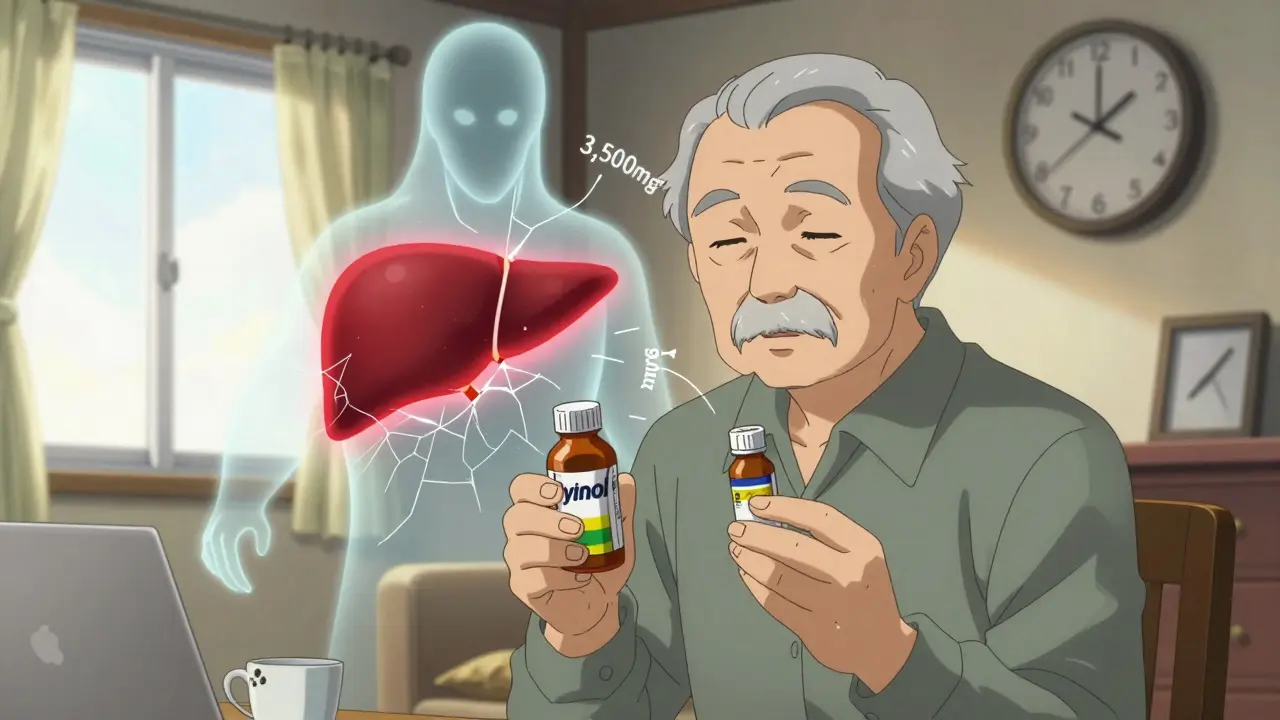
Acetaminophen (Tylenol) is different. It reduces pain and fever but doesn’t touch inflammation. That’s why it’s often the go-to for headaches or fever in kids and older adults. But here’s the catch: it’s processed by the liver. Take too much - even just a few extra tablets over a few days - and you can cause serious liver damage. In fact, acetaminophen overdose is the leading cause of acute liver failure in the UK and US.
Antihistamines fall into two camps. First-gen ones like diphenhydramine (Benadryl) knock you out. They work fast, but drowsiness is guaranteed - and that’s dangerous if you’re driving or operating machinery. Second-gen options like loratadine (Claritin) and cetirizine (Zyrtec) don’t cause sleepiness for most people. They last 24 hours and are safer for daily use. But they’re not magic. Some people still feel foggy, and older adults are at higher risk for confusion or falls.
How Much Is Too Much? Dosing Limits You Can’t Ignore
Most people don’t realize how easy it is to accidentally overdose. Let’s break it down.
- NSAIDs: Maximum daily dose for ibuprofen is 1,200mg (six 200mg tablets). Don’t take it for more than 10 days straight without checking with a pharmacist. Naproxen (Aleve) maxes out at 660mg per day. Aspirin (also an NSAID) shouldn’t be used daily unless advised - it increases bleeding risk.
- Acetaminophen: The official max is 4,000mg per day. But many doctors now recommend staying under 3,000mg. Why? Because many cold and flu meds also contain acetaminophen. You might take Tylenol for a headache, then grab a cold tablet - and suddenly hit 3,500mg before lunch. That’s dangerous.
- Antihistamines: Loratadine (Claritin) and cetirizine (Zyrtec) are 10mg once daily. Don’t double up. Diphenhydramine (Benadryl) is 25-50mg every 4-6 hours, but don’t use it more than 3 days in a row. It builds tolerance fast and can cause next-day grogginess.
Here’s a real scenario: A 58-year-old man takes one Tylenol for a headache, then takes a cold tablet at night because he’s got a runny nose. That cold tablet has 325mg of acetaminophen. He does this for three days. By day four, he’s taken 2,600mg just from those two products - and he hasn’t even touched the painkillers for his back. That’s how liver damage creeps up quietly.
Who Should Avoid These Meds - And Why
Not everyone can safely use these drugs. Here’s who needs to be extra careful.
- NSAIDs: Avoid if you have stomach ulcers, kidney disease, high blood pressure, or heart failure. They can raise blood pressure and worsen kidney function. Asthmatics should also steer clear - about 15% of people with asthma have severe reactions to NSAIDs.
- Acetaminophen: If you drink alcohol regularly (even one drink a day), your liver is already under stress. Combining it with acetaminophen increases liver damage risk by 300%. Also, don’t use it if you have severe liver disease.
- Antihistamines: First-gen antihistamines like Benadryl are risky for anyone over 65. They can cause confusion, urinary retention, and increase fall risk by nearly half. Even second-gen versions like Zyrtec can affect older adults differently. Always check with a pharmacist if you’re on other meds.
Why One Person’s Relief Is Another’s Nightmare
Some people swear by ibuprofen for their period cramps. Others can’t touch it - their stomach rebels. That’s because genetics play a role. A 2023 study found that 20% of people respond better to one antihistamine over another due to how their body processes histamine. Same with pain meds. Your body’s enzymes handle NSAIDs and acetaminophen differently than your neighbour’s.
That’s why trial and error is part of the process. If one painkiller gives you stomach pain, try acetaminophen. If it makes you drowsy, switch to a second-gen antihistamine. But don’t keep guessing without limits. If you’re using OTC meds for more than 10 days a month, you’re masking a bigger problem.
Hidden Dangers: Combination Products and Silent Overdoses
One of the biggest mistakes? Not reading labels. Many cold, flu, and sleep aids contain acetaminophen or antihistamines. You might think you’re taking just one thing - but you’re actually stacking drugs.
For example:
- DayQuil + Tylenol = double acetaminophen
- Allegra + Benadryl = double antihistamine
- Advil PM + Tylenol = NSAID + acetaminophen combo
The FDA says 20% of pediatric overdoses happen because parents confuse teaspoons (tsp) with tablespoons (tbsp). Liquid Tylenol is 160mg per 5mL - a tablespoon is three times that. A measuring cup isn’t enough. Always use the syringe or cup that comes with the bottle.
Also, store brands aren’t always cheaper in the long run. Generic ibuprofen works the same as Advil. But some store brands cut corners on inactive ingredients - and if you’re allergic to dyes or fillers, that’s a problem. Check the label for “inactive ingredients” if you’ve had reactions before.

When to Stop and See Someone
OTC meds are great for short-term relief. But if you’re using them too often, it’s a red flag.
Stop and call a pharmacist or doctor if:
- You need pain relief more than 10 days a month
- You’re taking more than one OTC painkiller at once
- You feel nauseous, yellowing skin, dark urine, or confusion after taking acetaminophen
- You get stomach pain, black stools, or dizziness after NSAIDs
- Your allergies aren’t improving after 7 days of antihistamines
Chronic pain or allergies aren’t meant to be managed with pills you grab off the shelf. There are better, safer long-term solutions - and your body is telling you it’s time to find them.
Smart Habits for Safe OTC Use
- Keep a log: Write down what you took, when, and why. It helps you spot patterns.
- Use the lowest effective dose. Don’t take two tablets if one works.
- Never mix alcohol with acetaminophen or first-gen antihistamines.
- Check expiration dates. Old meds lose potency - and can break down into harmful compounds.
- Ask your pharmacist. They see hundreds of OTC users every week. They know which products are safest for your age, meds, and health history.
And if you’re unsure? Skip the guesswork. Walk into a pharmacy. Show them your bottle. Ask: “Is this safe for me?” It takes 5 minutes. It could save your liver.
Can I take ibuprofen and acetaminophen together?
Yes, you can take them together - but only if you stick to safe doses. For example, 400mg ibuprofen and 650mg acetaminophen every 6 hours is generally safe for healthy adults. But don’t do it daily. This combo is meant for short-term flare-ups, not long-term use. Always space them out - don’t take them at the same time. And if you’re over 65, have kidney or liver issues, or take other meds, talk to a pharmacist first.
Is Tylenol safer than ibuprofen?
It depends. Tylenol (acetaminophen) is safer for your stomach and doesn’t affect blood pressure or kidney function like NSAIDs do. But it’s harder on your liver. If you have liver disease, drink alcohol, or take other liver-metabolized drugs, Tylenol is riskier. If you have ulcers, asthma, or high blood pressure, ibuprofen is riskier. Neither is universally “safer.” Choose based on your health history - not marketing.
Why do some antihistamines make me sleepy and others don’t?
First-gen antihistamines like diphenhydramine (Benadryl) cross the blood-brain barrier and block histamine in your brain - which causes drowsiness. Second-gen ones like loratadine (Claritin) and fexofenadine (Allegra) are designed not to enter the brain. That’s why they don’t make you sleepy. But everyone’s different. Some people still feel foggy on second-gen meds due to genetics, age, or other medications they’re taking.
Can I take OTC meds every day for allergies?
Second-gen antihistamines like loratadine, cetirizine, and fexofenadine are safe for daily use - even for months at a time. But if you’re still sneezing, itchy, or congested after 7-10 days, you need more than pills. You might have nasal polyps, a sinus infection, or environmental triggers you haven’t addressed. Talk to a doctor. Daily antihistamines mask symptoms - they don’t fix the cause.
What’s the safest OTC painkiller for seniors?
For most older adults, acetaminophen (Tylenol) is the safest first choice - if they don’t drink alcohol or have liver disease. NSAIDs increase fall risk, kidney strain, and bleeding. Antihistamines cause confusion. But even acetaminophen needs caution: limit to 3,000mg per day, never combine with other meds containing it, and always use the lowest dose that works. Always check with a pharmacist before starting any daily medication.



Robert Petersen
February 10 2026I used to pop ibuprofen like candy until my stomach started rebelling. Switched to acetaminophen and thought I was golden... until I learned about the liver thing. Now I keep a little logbook - what I took, why, and when. Best habit I ever picked up. Seriously, if you're using OTC meds more than a few days a week, you're not fixing the problem - you're just hiding it.