Nausea Tracker & Prevention Tool
Daily Nausea Log
Patterns & Insights
Key Insights
Getting sick from your medicine shouldn’t be part of the deal. If you’ve ever taken a pill and immediately felt like you were going to throw up, you’re not alone. Medication-related nausea and vomiting affect millions of people every year - not just cancer patients, but anyone on antibiotics, painkillers, antidepressants, or even daily vitamins. The good news? You don’t have to just endure it. There are clear, proven ways to stop it before it starts - and to calm it down when it does.
Why Do Medications Make You Nauseous?
It’s not random. Your body reacts to certain drugs in predictable ways. Some medications irritate your stomach lining directly - think NSAIDs like ibuprofen or aspirin. Others trigger your brain’s vomiting center through the chemoreceptor trigger zone, which is especially common with chemotherapy, opioids, and some antibiotics. Even SSRIs, often prescribed for anxiety or depression, can cause nausea because they boost serotonin, a chemical that’s closely tied to nausea signals. The worst part? Nausea often hits hardest right after you start a new drug. That’s when your body hasn’t adjusted yet. And if you don’t manage it early, it can turn into a cycle: you feel sick, you skip your dose, your condition gets worse, and you end up back at the doctor’s office.First Line of Defense: Simple, Non-Drug Fixes
Before you reach for a prescription antiemetic, try these low-cost, no-side-effect strategies. They work for most people - and they’re backed by cancer centers, pharmacies, and patient surveys.- Take meds with food. Unless your doctor says otherwise, eat something light before you take your pill. Antibiotics, NSAIDs, iron supplements, and multivitamins all cause less nausea when swallowed with a small snack - even a few crackers or a banana. This simple step cuts nausea in half for many.
- Eat small, frequent meals. Big meals overwhelm your stomach when it’s already sensitive. Instead of three large meals, try five or six tiny ones. Focus on bland, easy-to-digest carbs: toast, rice, oatmeal, plain pasta. Avoid greasy, spicy, or overly sweet foods - they make nausea worse.
- Stay hydrated, but sip slowly. Dehydration makes nausea feel worse. Drink water, clear broths, or electrolyte drinks in small sips. Chugging makes it worse. Ice chips or frozen fruit pops can help if you can’t keep liquids down.
- Try ginger. It’s not just a home remedy. Multiple studies show ginger reduces nausea from chemotherapy, motion sickness, and even pregnancy. Ginger chews, tea, or capsules (250-500 mg every 2-4 hours) have helped patients drop their nausea from an 8/10 to a 3/10 in less than a day.
- Get fresh air. Stuffy rooms and strong smells can trigger vomiting. Open a window. Step outside. Even sitting near a fan can help. Cool air calms the nausea center in your brain.
- Avoid your favorite foods during treatment. If you eat your favorite meal and then throw up, your brain will link that food to feeling sick. Next time you smell it, you’ll feel nauseous again - even if the drug isn’t the cause anymore. This is called conditioned nausea, and it’s real.
When You Need Medicine to Stop the Nausea
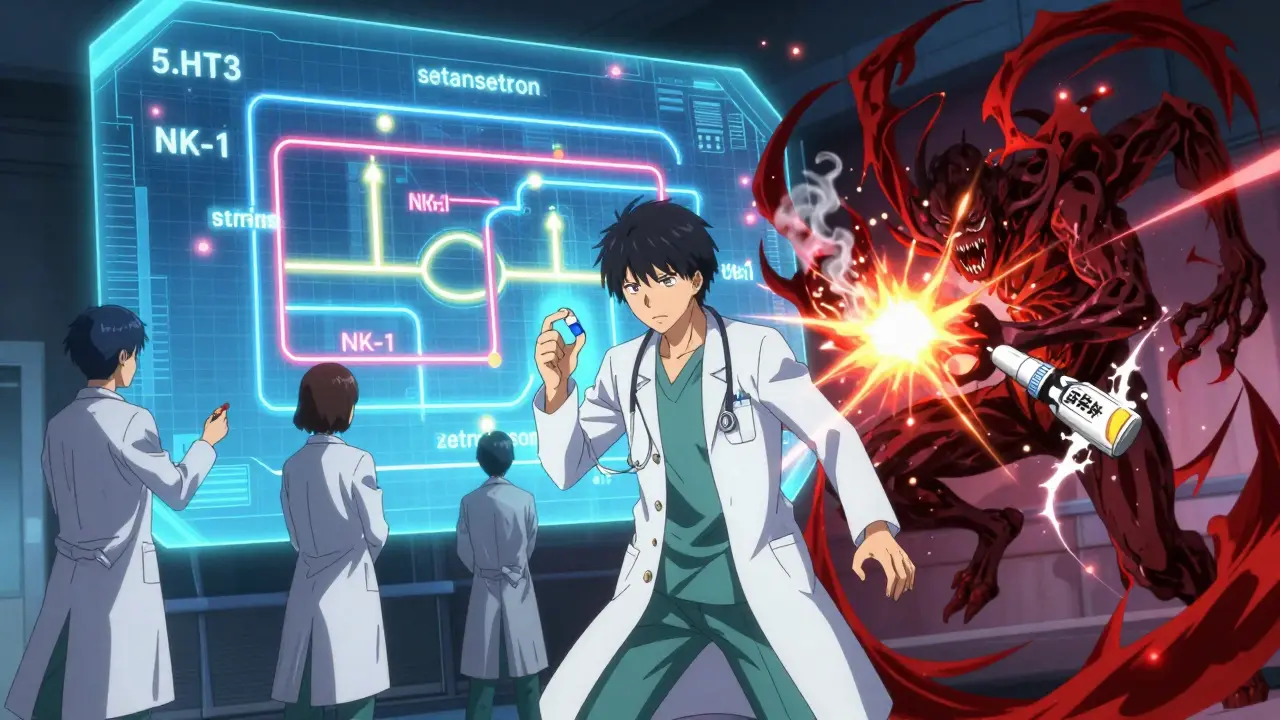
If simple fixes don’t cut it, it’s time to talk about anti-nausea drugs. These aren’t all the same. Each works on a different part of your body’s vomiting system.- 5-HT3 blockers (ondansetron, granisetron): These are the most common. Ondansetron (Zofran) blocks serotonin in your gut and brain. It’s effective for chemo, post-op nausea, and even some drug-induced vomiting. A single 4-8 mg dose can reduce vomiting by 60-70%. It’s available as a pill, a dissolving strip, or an injection.
- NK-1 blockers (aprepitant, rolapitant): These are stronger and used for severe cases, especially with chemotherapy. They work alongside 5-HT3 blockers for a one-two punch. When combined with dexamethasone, they can stop nausea and vomiting in 75-85% of patients. They’re more expensive - often $150-$300 per dose without insurance - but worth it for high-risk treatments.
- Mirtazapine: Originally an antidepressant, it’s now used off-label for nausea because it blocks serotonin receptors too. At low doses (15-30 mg), it helps with post-surgery nausea and even chronic nausea from conditions like gastroparesis. It also helps with sleep, which is a bonus for people who can’t rest because they’re nauseous.
- Low-dose tricyclic antidepressants (nortriptyline, amitriptyline): These aren’t for everyone. They help with long-term functional nausea - the kind that lasts for months with no clear cause. One study found 51% of patients had complete relief. But they don’t work for acute nausea from chemo or antibiotics. And they can cause drowsiness or dry mouth.
Important note: Not all anti-nausea drugs work for every situation. For example, 5-HT3 blockers like ondansetron are great for vomiting, but less so for nausea alone. That’s why some patients still feel queasy even after taking them. That’s when you need to combine approaches.
Special Cases: Chemo, Surgery, and Anticipatory Nausea
Different triggers need different plans.Chemotherapy: The standard is a three-drug combo - an NK-1 blocker, a 5-HT3 blocker, and dexamethasone. This is called triplet therapy. For moderate-risk chemo, two drugs (5-HT3 + dexamethasone) are enough. If you’re getting chemo, ask your oncologist which category your drug falls into. Don’t assume you need the strongest meds.
Post-surgery nausea: Women and non-smokers are at higher risk. The latest guidelines recommend giving dexamethasone and ondansetron before you wake up. A study found that patients who got both IV and oral ondansetron before leaving the hospital had 23% less nausea at home than those who only got the IV shot. That’s a big difference.
Anticipatory nausea: This is when you start feeling sick just thinking about your next treatment. It’s psychological, not physical. Drugs don’t help much here. Instead, cognitive behavioral therapy (CBT) works. A 2022 position paper from the American Psychosocial Oncology Society says CBT should be offered to every patient with this issue. Breathing exercises, guided imagery, and even hypnosis can break the mental link between the clinic and nausea.
What Not to Do
Some common “solutions” make things worse.- Don’t skip doses. One in three patients reduces or stops their medication because of nausea - without telling their doctor. That can make their original condition worse. If you’re struggling, talk to your provider. There’s almost always a better way.
- Don’t use metoclopramide long-term. It’s an older drug that speeds up stomach emptying. But if you take it for more than 12 weeks, you risk a serious movement disorder called tardive dyskinesia. It’s not worth the risk unless other options fail.
- Don’t rely on alcohol or caffeine. Both dehydrate you and irritate your stomach. They might seem like they help at first, but they’ll make nausea worse later.
How to Talk to Your Doctor
Don’t wait until you’re miserable. When you start a new medication, ask these questions:- Is nausea a common side effect of this drug?
- Should I take it with food or on an empty stomach?
- Is there a lower dose I can start with to build tolerance?
- Do you recommend any anti-nausea medicine to take with this?
- What should I do if the nausea doesn’t improve after a few days?
Bring up cost too. If a drug like aprepitant is priced at $250 per dose and you don’t have good insurance, ask if there’s a generic alternative or a patient assistance program. Many drugmakers offer free or discounted meds for people who qualify.
Tracking Your Progress
Write down your symptoms. Use a simple scale: 0 = no nausea, 10 = worst ever. Note what you ate, what meds you took, and what helped. Many cancer centers now use apps like Nausea Tracker to log this data. Even a paper journal works. Patterns emerge fast - you might notice nausea spikes every time you take your pill after 2 p.m., or after eating dairy. That’s information your doctor can use to adjust your plan.Follow-up matters. Check in at 24 hours, 72 hours, and 7 days after starting a new drug. If nausea hasn’t improved by then, it’s time to change tactics. Waiting too long can turn a manageable side effect into a reason to quit treatment entirely.
What’s New in 2026
The field is evolving. In 2023, the FDA approved rolapitant for kids as young as 2 - a big win for pediatric cancer care. New drugs like HTL0022261 are in late-stage trials and may offer fewer heart-related risks than older 5-HT3 blockers. Digital tools are also expanding: apps that remind you to take your anti-nausea meds, track your food intake, or guide you through breathing exercises are now used in 42% of top cancer centers.The future isn’t just about better drugs. It’s about personalization. Scientists are studying how your genes affect how you respond to antiemetics. One day, a simple blood test might tell your doctor which nausea drug will work best for you - before you even take the first pill.
Can I take ginger with my prescription anti-nausea medicine?
Yes, ginger is generally safe to use with most anti-nausea medications like ondansetron or mirtazapine. Studies show it works through different pathways than drugs, so it often enhances their effect. Stick to 250-500 mg of ginger root extract every 2-4 hours. Avoid high doses (over 1,000 mg daily) if you’re on blood thinners, as ginger can have mild anticoagulant effects.
Why does my nausea get worse at night?
Lying down slows digestion and can cause stomach acid to rise, making nausea worse. Also, if you took your medication right before bed, your body may be processing it while you’re asleep. Try taking your pill earlier in the evening, or ask your doctor if switching to a nighttime dose (like with SSRIs) might help. Elevating your head with an extra pillow can also reduce reflux-related nausea.
Is it safe to use over-the-counter anti-nausea meds like Pepto-Bismol with prescription drugs?
Pepto-Bismol (bismuth subsalicylate) is usually safe for occasional use, but it can interact with blood thinners, gout medications, and some antibiotics. It’s also not effective for nausea caused by brain-based triggers like chemo or opioids. For drug-induced nausea, stick to proven options like ondansetron or ginger. Always check with your pharmacist before combining OTC and prescription meds.
How long does medication-induced nausea usually last?
It depends on the drug. For antibiotics or NSAIDs, nausea often fades within 3-7 days as your body adjusts. With chemotherapy, acute nausea peaks within 24 hours and can last up to 5 days. Delayed nausea can stretch to a week or more. If nausea lasts longer than 10 days after starting a new medication, talk to your doctor - it could be a sign of another issue, like an infection or liver problem.
Can stress make medication nausea worse?
Absolutely. Stress activates the same brain pathways involved in nausea. If you’re anxious about side effects, your body may amplify them. Techniques like deep breathing, mindfulness, or even listening to calming music can reduce nausea intensity by 20-40%. For chronic nausea, combining relaxation practices with medication gives better results than either alone.



Saylor Frye
January 7 2026Look, I get it - ginger’s cute and all, but if you’re on chemo and think a $5 tea bag is gonna replace Zofran, you’re living in a Whole Foods fantasy. This isn’t ‘wellness’ - it’s pharmacology. Stop romanticizing folk remedies and start talking to your oncologist like an adult.
Kelly Beck
January 7 2026OMG YES!! 🙌 I was so sick on my new antidepressant and thought I’d have to quit… then I tried ginger chews + eating crackers before bed 🥹 and like… 3 days later I was actually sleeping?!? My therapist said I was ‘reclaiming my body’ and I cried in the shower 😭 thank you for validating what felt like a personal failure!! 💕
Joann Absi
January 8 2026They don’t want you to know this but Big Pharma HATES ginger because it’s FREE and doesn’t need a patent. They push Zofran because it’s $800 a pill and your insurance pays for it while you bleed out in debt. Wake up, sheeple! The FDA is just a shell corporation for Pfizer. I’ve been off all meds for 3 years now and I’m healthier than ever - just lemon water, sunlight, and willpower. 🇺🇸🔥
Mukesh Pareek
January 9 2026From a clinical pharmacology standpoint, the 5-HT3 antagonism pathway is well-documented, but the efficacy of ginger (Zingiber officinale) is mediated via TRPV1 and 5-HT3 receptor modulation, which is dose-dependent and exhibits a U-shaped curve. Most patients underdose - 250 mg is subtherapeutic for chemo-induced nausea. You need 1 g TID minimum, and even then, bioavailability is poor without piperine co-administration. Also, avoid concurrent NSAIDs - they upregulate COX-2 and exacerbate gastric irritation.
Jeane Hendrix
January 11 2026wait so if i take my ssri with food and then drink ginger tea and then sleep with my head propped up… does that count as a ‘protocol’?? 😅 i’ve been doing all these things but i’m still dizzy and my brain feels like wet cotton… is this normal?? or am i just doing it wrong??
Tom Swinton
January 12 2026I just want to say - this article saved my life. Seriously. I was on antibiotics for a sinus infection and couldn’t keep anything down for five days - I thought I was dying. I tried the crackers, the ginger tea, the fresh air… and by day three, I was actually eating again. I cried. I’m not even joking. I felt like I’d been given back my body. Thank you for writing this. You’re not just giving advice - you’re giving hope. 🙏💛
Gabrielle Panchev
January 14 2026Wait… so you’re telling me… that if I take my meds with food… I won’t throw up…? And that ginger… works…? And that I shouldn’t skip doses…? This is the most radical, dangerous, anti-capitalist, pro-body, anti-pharma, pro-common-sense article I’ve ever read. Are you sure this isn’t a CIA psyop? I mean… why would Big Pharma ever want us to know that simple things work? This is too easy. Too… logical. I’m suspicious.
Melanie Clark
January 14 2026They told me to take ginger and eat crackers but I know the truth. The government has been poisoning our water with lithium to make us feel nauseous so we’ll buy more antidepressants. The FDA knows. The WHO knows. Even my pharmacist winked when I asked about Zofran. I stopped all meds. I drink rainwater. I sleep on a copper mat. I feel better. I’m not sick. I’m awake.
Vinayak Naik
January 15 2026bro i took azithromycin and felt like my stomach was trying to crawl out my throat… then i tried the ginger thing - 500mg capsule with a spoon of honey - and like… 20 mins later i was watching netflix like nothing happened. also, dont forget: if you take meds at night, your stomach is lazy and everything sits there like a rock. i started taking mine at 7am and life changed. also, if you’re indian, try ajwain seeds - they’re like ginger’s spicy cousin. cheap, everywhere, and works like magic. 🙏