Every household has medications-prescription pills, over-the-counter pain relievers, creams, inhalers, even supplements. But how many of us actually know where they’re stored, if they’re still good, or if a child could reach them? A simple medication storage checklist can prevent poisonings, mix-ups, and wasted drugs. It’s not about being overly cautious. It’s about making sure the medicine you rely on works when you need it-and doesn’t hurt someone by accident.
Start with Where You Store It
The bathroom cabinet is the most common place people keep meds. But it’s also the worst. Showers create humidity spikes up to 90%, and the temperature jumps 10-15 degrees with every hot water use. That kind of environment breaks down pills and liquids faster. The FDA says some medications lose up to 40% of their potency after just 30 days of light and moisture exposure.
Instead, pick a dry, cool, and consistent spot. A linen closet, a drawer in a bedroom dresser, or a small cabinet in a powder room works best. These areas stay between 68-77°F and humidity stays around 40-50%. Keep meds away from windows, radiators, and appliances that heat up. If you’re unsure, use a simple indoor thermometer and hygrometer-both cost less than £15 online. Check them once a week.
Separate Medications by Person and Type
Keeping everyone’s meds together is a recipe for mistakes. A 2022 study in the Journal of Patient Safety found that separating prescriptions by household member cuts accidental mix-ups by 63%. That means no more grabbing your partner’s blood pressure pill because yours ran out.
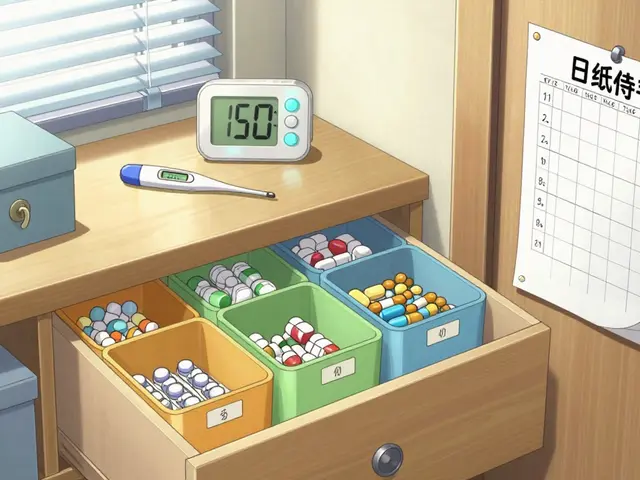
Use different shelves, bins, or even colored containers. Label each section clearly: “John’s Prescriptions,” “Sarah’s OTCs,” “Topicals.” This also helps if someone has trouble reading small print. Don’t mix pills and creams. A 2021 FDA report documented 127 cases where topical ointments were mistakenly swallowed because they were stored in the same container as oral meds.
High-risk drugs like insulin, warfarin, or opioids need extra care. Store them in their own locked container, even inside the main storage area. Label it clearly: “High Alert.” A 2020 Ontario pilot study showed this simple step reduced dosing errors by 78%.
Lock It Down-Especially If Kids or Teens Are Around
Standard medicine cabinets? They’re useless against curious kids. The Consumer Product Safety Commission tested 100 cabinets and found only 12% blocked children under 5. That’s why the EPA recommends locked cabinets, safes, or dedicated medicine lockboxes.
A 2023 Pediatrics study showed households using lockboxes saw 92% fewer accidental ingestions in children under 5. Combination locks are 34% more reliable than key locks-no one forgets a code. Keep meds at least 4 feet off the ground and behind three closed doors if possible. That’s the setup used in childcare centers under North Carolina’s Kaitlyn’s Law, and it reduced child access by 88%.
Teens are another risk. Thirty percent of teens who misuse prescription drugs get them from home medicine cabinets. A locked box doesn’t just protect them from others-it protects others from them.

Check Expiration Dates Every Six Months
Most people don’t know when their meds expire. The BeMedWise organization found that 70% of homes have at least one expired medication. But here’s the thing: many pills still work after their expiration date. The FDA says 82% retain at least 90% potency one year past expiry-if stored properly. But at three years, that drops to 42%.
Don’t wait for the bottle to look strange. Set a calendar reminder every six months. Do it when you change the clocks for daylight saving time-it’s a built-in habit. Look for:
- Color changes (pills turning yellow or brown)
- Texture changes (crumbly tablets, sticky liquids)
- Unusual smells (sour, chemical, or rotten odors)
If you see any of these, throw it out. Don’t risk it. For multi-dose vials like insulin or eye drops, write the date you opened them. Most lose effectiveness after 28-56 days, even if the bottle says otherwise.
Special Rules for Special Medications
Not all meds are created equal. Insulin must be refrigerated until opened (36-46°F). Once opened, it can stay at room temperature for up to 56 days, depending on the type. But if you leave it on the counter in direct sunlight? Potency drops by 30%.
Inhalers? Store them in their original plastic case to prevent accidental spray. Moisture can clog the nozzle. A 2023 BeMedWise report found 22% of users had device failures due to improper storage.
Topical creams, sunscreens, insect repellents, and even nutritional supplements? They count as medications under Kaitlyn’s Law. Keep them in original containers with labels. A 2019 UNC Chapel Hill study showed this reduced errors by 72% in homes with young children.

Dispose of Expired or Unwanted Meds the Right Way
Flushing meds down the toilet or throwing them in the trash? That’s outdated-and dangerous. The EPA says 60-80% of pharmaceuticals flushed into water systems end up in rivers and drinking water. The USGS detected drug residues in 80% of U.S. waterways.
Use a drug take-back program. The DEA’s National Prescription Drug Take Back Day collects over a million pounds of meds each year. Check your local pharmacy or police station-they often have year-round drop boxes.
If no take-back is available, mix pills with something unappealing: coffee grounds, cat litter, or dirt. Put them in a sealed container before tossing. A 2020 FDA study showed this cuts accidental ingestion by 76%. Never leave empty bottles or loose pills lying around.
Build Your Routine
A checklist only works if you use it. Here’s how to make it stick:
- Monthly: Do a quick visual check. Look for mold, discoloration, or leaks.
- Every 3 months: Verify all labels are legible. Replace faded stickers.
- Every 6 months: Clear out expired meds. Use the daylight saving time change as your reminder.
- Daily: If you store meds in the fridge, check the temperature. It should be 36-46°F. Keep a log for 30 days-you’ll spot fluctuations before they ruin your meds.
Households with a formal storage system have 89% fewer medication-related incidents, according to a 2023 Consumer Reports survey. That’s not luck. That’s structure.
What to Do If Something Goes Wrong
Accidents happen. If a child swallows a pill, call Poison Control immediately: 1-800-222-1222 (U.S.) or 111 (UK). Don’t wait for symptoms. If an adult takes the wrong med, bring the bottle and the person to the ER. Don’t guess what it was.
Keep a printed copy of your checklist in the storage area. That way, if someone else needs to check it-like a visiting nurse or family member-they know exactly what’s where.
Where’s the best place to store medications at home?
The best place is a dry, cool, and consistent spot away from moisture and heat. Avoid bathrooms and kitchens. A linen closet, a bedroom drawer, or a locked cabinet in a hallway works best. Keep the temperature between 68-77°F and humidity under 50%. Use a simple thermometer and hygrometer to monitor conditions.
Should I keep all medications in the fridge?
Only if the label says so. Most meds don’t need refrigeration. Insulin must be refrigerated until opened, then can stay at room temperature for up to 56 days. Other meds like eye drops or certain antibiotics may need cold storage. Always follow the manufacturer’s instructions. Storing non-refrigerated meds in the fridge can cause condensation and damage them.
How often should I check for expired medications?
Check every six months. Set a reminder for the same time each year-like when daylight saving time changes. This helps you catch expired pills before they’re taken. Don’t wait for them to look bad. Many degrade without visible signs. Discard anything past its expiration date, especially if it’s changed color, texture, or smell.
Can I flush old pills down the toilet?
No. Flushing meds pollutes water systems. The EPA says 60-80% of pharmaceuticals flushed into sewers end up in rivers and drinking water. Instead, use a drug take-back program at a pharmacy or police station. If none are available, mix pills with coffee grounds or cat litter in a sealed container before throwing them in the trash.
What if I have a child or elderly person living with me?
Lock all medications in a secure container. Use a lockbox with a combination, not a key. Store meds at least 4 feet off the ground and behind closed doors. Separate each person’s meds clearly. Elderly individuals often confuse similar-looking bottles-labeling with large print helps. Consider using a pill organizer with alarms if someone forgets doses.
Are over-the-counter meds and supplements included in a medication checklist?
Yes. The North Carolina Kaitlyn’s Law defines medications broadly to include OTC drugs, topical creams, repellents, and even nutritional supplements. All of them can be harmful if misused or taken incorrectly. Store them with your other meds and include them in your six-month inventory.