When you see bright red blood in your stool, it’s scary. You might think it’s just hemorrhoids. But if you’re over 60, it could be something more serious-like diverticula bleeding or angiodysplasia. These two causes account for nearly half of all lower GI bleeds in older adults. And while many cases stop on their own, others need quick, precise diagnosis and treatment. This isn’t about guesswork. It’s about knowing what to look for, when to act, and how doctors find the source.
What Exactly Is Lower GI Bleeding?
Lower gastrointestinal bleeding means blood is coming from your colon, rectum, or anus-anywhere past the ligament of Treitz, which marks the end of the small intestine. The most common sign? hematochezia: bright red or maroon blood mixed with stool. Sometimes it’s just streaks on the toilet paper. Other times, it’s a full gush. Unlike upper GI bleeds that cause black, tarry stools (melena), lower GI bleeds usually don’t hurt. That’s why they’re easy to ignore-until you’re lightheaded or weak from blood loss.About 20 to 33% of all GI bleeds are lower. Each year, 20 to 27 people out of every 100,000 experience it. Most are over 60. And while hemorrhoids and anal fissures are common, they’re not the whole story. In fact, when someone ends up in the hospital with a major bleed, the top two culprits are diverticula and angiodysplasia.
Diverticula: The Silent Bleeders
Diverticula are small pouches that bulge out from the colon wall. They’re super common-nearly half of people over 60 have them. Most never cause problems. But when one of the tiny blood vessels running near the pouch ruptures, you get diverticular bleeding.This isn’t diverticulitis. There’s no fever, no cramping, no inflammation. It’s just a vessel that pops. And when it does, the bleed can be massive. People often describe it as a sudden, painless flood of blood. One minute you’re fine. The next, you’re sitting in a pool of red.
Why does it happen? The blood vessels that feed the colon run through the muscle layer. As diverticula form, these vessels get stretched over the top of the pouch. They’re thin, exposed, and fragile. A little pressure-maybe from straining or even normal bowel movement-and they tear. About 30 to 50% of hospitalizations for lower GI bleeding are due to this.
Good news? About 80% of these bleeds stop on their own. But that doesn’t mean you can wait. Even if the bleeding stops, you need to know it was diverticula and not something worse-like cancer. That’s why doctors don’t just assume.
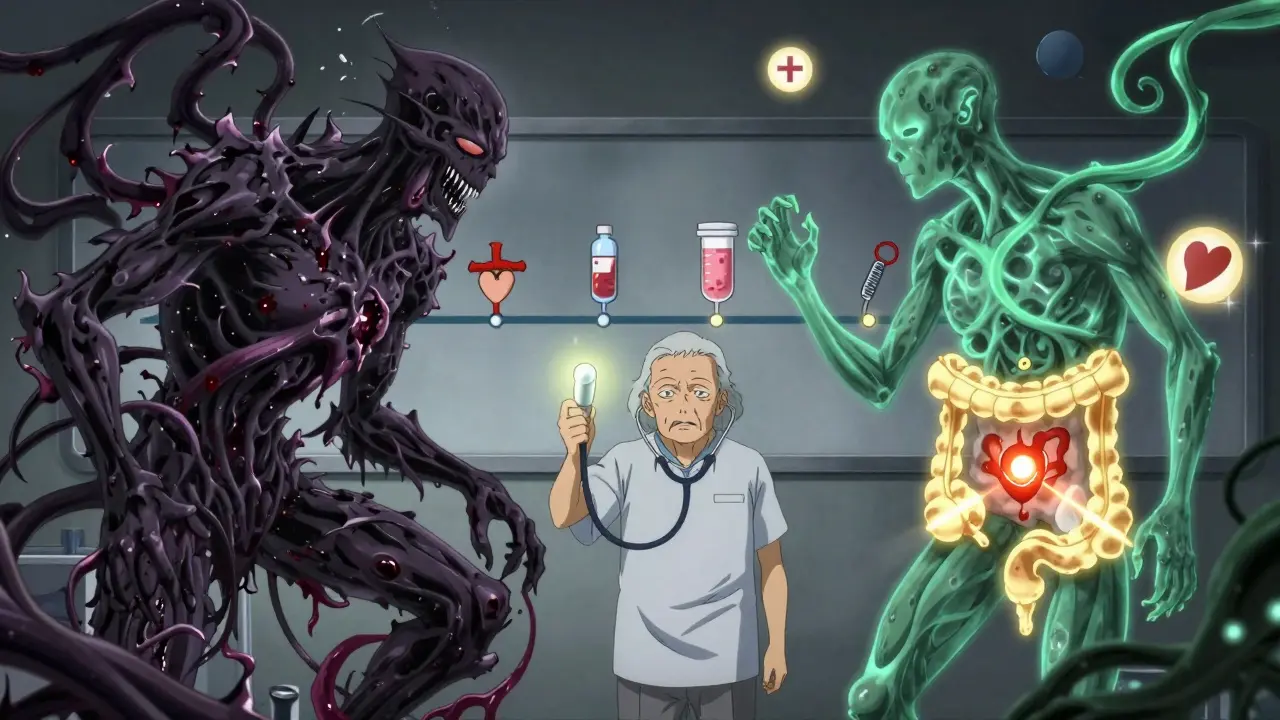
Angiodysplasia: The Slow Leak
If diverticula are the sudden flood, angiodysplasia is the slow drip. Also called vascular ectasia or AVMs (arteriovenous malformations), these are tangled clusters of tiny blood vessels in the colon lining. They’re most common in the right side of the colon-the cecum and ascending colon.These aren’t birth defects. They develop over time. As you age, the normal motion of your colon puts constant pressure on these vessels. They stretch, thin out, and form weak connections between arteries and veins. Think of it like a garden hose that’s been kinked for years-eventually, it starts to leak.
Unlike diverticula, angiodysplasia rarely causes big, dramatic bleeds. Instead, it leaks slowly. You might notice dark red streaks in your stool, or just feel tired, short of breath, or dizzy. That’s because you’re slowly losing iron. Many patients are diagnosed only after a routine blood test shows severe anemia-hemoglobin under 10 g/dL.
It’s most common in people over 65. The average age at diagnosis? 72. And here’s a key detail: if you have aortic stenosis (a narrowed heart valve), your risk goes up. Turbulent blood flow through that valve breaks down a clotting protein called von Willebrand factor. Without it, even small vessels bleed more easily.
Doctors sometimes mistake angiodysplasia for simple anemia. But if you’re over 65, have unexplained iron deficiency, and no other obvious cause-you need to look at your colon.
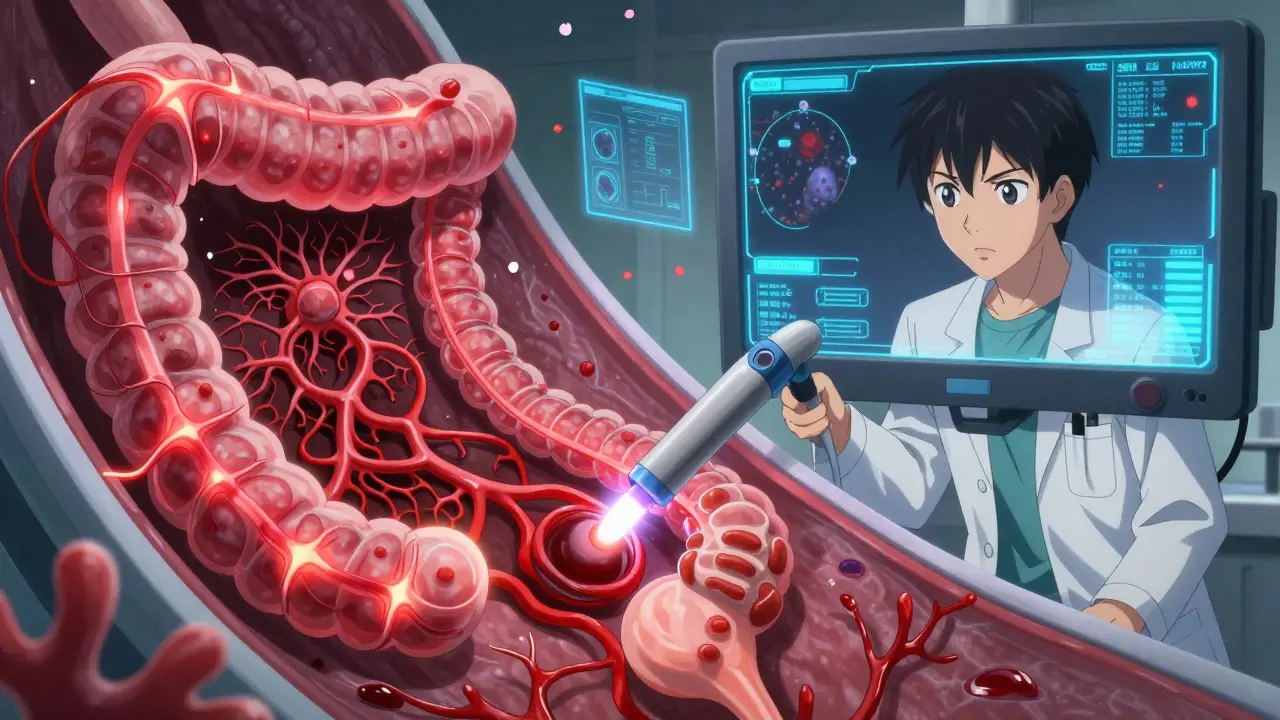
How Doctors Find the Source: The Workup
When someone walks in with GI bleeding, the first step isn’t scanning or scopes. It’s stabilization. Are they dizzy? Is their heart racing? Is their blood pressure low? If yes, they get fluids, oxygen, and possibly a blood transfusion. Then comes the real work: finding the source.The gold standard? Colonoscopy. Done within 24 hours of admission, it finds the bleeding site in over 80% of cases. And here’s the kicker-it can treat it too. You don’t just look. You stop the bleed.
But here’s the catch: if the colon is full of blood, it’s hard to see. That’s why doctors sometimes use a trick-give you IV fluids and a drug called erythromycin. It speeds up gut movement, clears out the blood and debris, and gives a clearer view. You don’t need a perfect prep like for a screening colonoscopy. Speed matters more than cleanliness.
What if the colon looks clean? Then the bleeding might be coming from higher up-small intestine or even the stomach. That’s when they turn to other tools:
- CT angiography: A special scan that shows active bleeding if it’s happening at a rate faster than half a milliliter per minute. It’s fast, non-invasive, and picks up about 85% of bleeding sites.
- Capsule endoscopy: You swallow a tiny camera. It takes pictures as it moves through your small intestine. It finds the cause in about 62% of cases where colonoscopy was negative. But it’s not perfect-15% of people have strictures (narrowing) they don’t know about, and the capsule can get stuck.
- Device-assisted enteroscopy: A longer scope that reaches deeper into the small bowel. It’s more invasive but has a 71% success rate. Only available in big hospitals with specialized teams.
Artificial intelligence is now helping too. New software can highlight subtle red spots on colonoscopy video that humans might miss-boosting angiodysplasia detection by 35%.
Treatment: What Happens After the Diagnosis
Once they find it, what do they do?For diverticula bleeding: If it’s stopped on its own, they watch. If it’s still bleeding, they go back in with a scope. The go-to method? Inject epinephrine (a vasoconstrictor) to shrink the vessel, then use heat (thermal coagulation) to seal it. Success rate? 85 to 90%. But here’s the problem: 20 to 30% of people bleed again. That’s why some now use new clipping devices-metal clips that clamp the vessel shut. One European study showed 92% success with those.
For angiodysplasia: The standard is argon plasma coagulation (APC). It’s like a jet of ionized gas that burns the abnormal vessels. Immediate stop? 80 to 90%. But recurrence? Up to 40% within two years. That’s why some patients end up back in the hospital multiple times.
For those with frequent rebleeds, there are two medical options:
- Thalidomide: A drug once used for morning sickness. Now it’s being used off-label for angiodysplasia. A 2019 trial in Gut showed it cut transfusion needs by 70%. But it has side effects-drowsiness, nerve damage, birth defects. Only for adults, only under close supervision.
- Octreotide: A hormone injection given under the skin three times a day. It tightens blood vessels. Works in about 60% of cases. Used more for patients who can’t have more endoscopy or surgery.
When all else fails? Surgery. For angiodysplasia in the right colon, they remove the right side of the colon (right hemicolectomy). For a single diverticulum that keeps bleeding, they remove just that segment.
Who’s at Highest Risk?
Not everyone with bleeding needs the same level of care. Doctors use a simple tool called the BLEED score to decide who’s in danger:- Blood pressure under 100
- Length of hospital stay over one day
- Endoscopic signs of recent bleeding
- Evidence of cancer or liver disease
- Diagnosis of diverticulosis or angiodysplasia
If you score high, you need urgent colonoscopy. If you’re over 70, have low blood pressure, and a hemoglobin under 9, you’re in the danger zone. Mortality for these patients? Up to 22% within 30 days. But that’s mostly because of heart disease, kidney failure, or other chronic illnesses-not the bleed itself.
For angiodysplasia, the death rate is lower-5 to 10%. But the real burden is quality of life. People with recurrent bleeding often go through years of tests, hospital visits, and transfusions. One patient group found that the average time from first symptoms to diagnosis was 18 months. And two out of three had three or more negative colonoscopies before the real cause was found.
What Happens After You’re Discharged?
You’re not done after the bleeding stops. You need follow-up.If it was diverticula, you’ll be told to eat more fiber. Not to prevent bleeding-because that doesn’t work-but to avoid constipation and straining. No need to avoid nuts or seeds. That old advice is outdated.
If it was angiodysplasia, you’ll likely need regular blood tests to check your iron and hemoglobin. Some patients take daily iron supplements. Others get periodic infusions. And if you have aortic stenosis, your cardiologist needs to know. Treating the heart valve can sometimes reduce GI bleeding.
Long-term survival? Good. Five-year survival is 78% for diverticular bleeding, 82% for angiodysplasia. But it’s not about the bleed. It’s about your other health conditions. Manage your heart, your kidneys, your blood pressure-and you’ll do fine.
What You Should Do If You See Blood
Don’t panic. But don’t ignore it either.- Call your doctor immediately if you see bright red blood in stool, especially if you’re over 60.
- Don’t wait for it to stop on its own. Even if it does, you need to know why.
- Bring a list of your medications-especially blood thinners, NSAIDs, or heart meds.
- If you’ve had anemia before, mention it. That’s a big clue.
- Ask: Could this be angiodysplasia? Could this be diverticula? Don’t let them dismiss it as hemorrhoids without ruling out the others.
Lower GI bleeding isn’t just a symptom. It’s a signal. And if you’re older, it’s often your body telling you something deeper is going on. The right diagnosis doesn’t just stop the bleeding-it changes your future.
Can diverticula bleeding be prevented?
No, you can’t prevent diverticula from forming-they’re a natural part of aging. But you can reduce the risk of rupture by avoiding constipation. Eat fiber-rich foods, drink water, and move regularly. Avoid straining during bowel movements. There’s no evidence that avoiding nuts, seeds, or popcorn helps.
Is angiodysplasia cancer?
No. Angiodysplasia is not cancer. It’s a vascular abnormality-like a weak, tangled blood vessel. But because it can cause bleeding and anemia, it’s often found during tests meant to rule out colon cancer. Doctors always check for tumors at the same time.
Why does angiodysplasia happen more in the right colon?
The right side of the colon has slower movement and higher pressure compared to the left. Over time, this constant pressure stretches the small blood vessels, making them more likely to form abnormal connections between arteries and veins. That’s why over 80% of cases are found in the cecum and ascending colon.
Can you have both diverticula and angiodysplasia at the same time?
Yes. Especially in older adults. It’s not uncommon to have both conditions. That’s why doctors don’t stop at the first finding. If you’ve had one bleed and the source is unclear, they’ll look again-because multiple causes can coexist.
What’s the best test for recurrent GI bleeding?
There’s no single best test. Colonoscopy comes first. If it’s negative, CT angiography is next because it’s fast and detects active bleeding. If bleeding is intermittent, capsule endoscopy is useful. For hard-to-find sources in the small bowel, device-assisted enteroscopy gives the highest yield-but only if available.
Does thalidomide really work for angiodysplasia?
Yes, but it’s not first-line. In a 2019 clinical trial, patients taking thalidomide (100 mg daily) needed 70% fewer blood transfusions compared to those on placebo. It’s used only when endoscopic treatments fail and bleeding keeps coming back. Side effects are serious, so it’s reserved for carefully selected patients under close supervision.
Can a colonoscopy miss angiodysplasia?
Yes. Angiodysplasias are small, flat, and often pale red. If the colon isn’t clean, or if the bleed has stopped, they can be missed. Even experienced endoscopists miss them up to 20% of the time. That’s why AI-assisted colonoscopy is changing things-it highlights subtle lesions humans overlook.

Harsh Khandelwal
December 25 2025So let me get this straight - they’re telling us to just sit there while our colon turns into a bloody horror show, and the solution is to shove a camera up our butt? And if that doesn’t work, they throw thalidomide at us? That’s the same drug they used to turn babies into mutant sea creatures in the 50s. I’m not dying because some doctor thinks my blood vessels are ‘tangled.’ I’m calling my lawyer after this.
Spencer Garcia
December 26 2025Great breakdown. Colonoscopy within 24 hours is critical - delay = higher risk. And yes, erythromycin prep is underused. It’s not about clean bowels, it’s about visibility. Also, AI detection of angiodysplasia? Huge leap. I’ve seen cases missed for years because the lesions were too subtle. This is medicine evolving.
Abby Polhill
December 26 2025Angiodysplasia is basically the colon’s version of varicose veins - just with more bleeding and less cute socks. The right colon’s slow flow + high pressure = perfect storm for vascular ectasia. And yeah, the von Willebrand factor degradation in aortic stenosis? Classic. I’ve seen three patients in my clinic this month with unexplained anemia - all had undiagnosed AS. Cardiologists need to talk to GI docs more.
Bret Freeman
December 27 2025They don’t want you to know this, but the real reason they push colonoscopies so hard is because Big Gastro makes billions off endoscopic clips and APC machines. And don’t get me started on thalidomide - that’s not medicine, that’s a last-ditch Hail Mary with side effects that turn you into a zombie. Meanwhile, the real cause? Processed food, glyphosate, and corporate greed. They’d rather inject you with chemicals than fix your diet.
Lindsey Kidd
December 28 2025Thank you for this. 💙 I’m 68 and had two episodes of bright red blood last year - thought it was hemorrhoids. Turns out, angiodysplasia. I’m on iron infusions now and feel like a new person. Please, if you’re over 60 and see red - don’t wait. It’s not ‘just aging.’ It’s your body screaming. Get checked. You deserve to feel good. 🌻
Rachel Cericola
December 29 2025Let’s be brutally honest - most primary care docs still treat lower GI bleeding like it’s a minor nuisance. They say ‘eat fiber’ and send you on your way. But if you’re over 65 with iron deficiency anemia and no obvious source, you’re not ‘just getting older,’ you’re bleeding internally. And if your hemoglobin is below 9 and you’re dizzy? That’s not a ‘maybe,’ that’s an ER visit. The BLEED score exists for a reason. Stop trusting gut feelings. Trust data. And if your doctor dismisses you? Find a new one. Your life isn’t a suggestion box.
Katie Taylor
December 29 2025THIS. This is the kind of info that saves lives. I’ve seen too many people die because they thought ‘it’ll stop.’ It doesn’t always. And the fact that AI is now catching what human eyes miss? That’s hope. Keep pushing this message. We need more clarity, not more fear. You did amazing work here.
Payson Mattes
December 31 2025Wait - so you’re telling me the government and Big Pharma don’t want us to know that diverticula are caused by GMO corn and fluoridated water? I’ve been researching this for 12 years. The real culprit is the sodium chloride in your toothpaste. It weakens the colon wall. And they hide it because they profit off colonoscopies. I’ve got the documents. Want to see them? I’ll DM you. Also, thalidomide was originally developed by Nazis. Coincidence? I think not.
Isaac Bonillo Alcaina
January 2 2026There is a fundamental flaw in your assertion that ‘diverticula are common in people over 60.’ This is statistically inaccurate. The prevalence is closer to 58%, not ‘nearly half.’ Additionally, you refer to ‘angiodysplasia’ as ‘AVMs’ - a misnomer. Arteriovenous malformations are congenital; angiodysplasias are acquired vascular ectasias. Your misuse of terminology undermines credibility. Furthermore, the BLEED score is not validated in patients with cirrhosis - you omitted this critical exclusion. This article reads like a blog post, not clinical guidance.
Joseph Manuel
January 3 2026The data presented is methodologically sound, though the narrative framing lacks academic rigor. The reliance on anecdotal patient descriptions ('sitting in a pool of red') introduces bias. While colonoscopy remains the gold standard, the sensitivity for angiodysplasia varies significantly based on endoscopist experience, bowel preparation quality, and lighting conditions - factors inadequately addressed. Furthermore, the claim that AI improves detection by 35% derives from a single-center study with small sample size. Until replicated in multicenter trials, this should be cited as preliminary.
Andy Grace
January 3 2026I’ve seen this play out in the bush clinics out here. Old blokes come in with pale skin and say, ‘It’s just a bit of blood, doc.’ They’ve been bleeding for months. We do a quick Hb test - 7.2. Then we send them 300 klicks to the city for a scope. By then, they’re in ICU. This post? It’s the kind of thing we need to print and stick on every GP’s wall. Thanks for saying it plainly.
Delilah Rose
January 5 2026I just want to say how much I appreciate how this post doesn’t just dump facts - it connects the dots between aging, physiology, and real human experience. I’m a nurse, and I’ve watched patients feel dismissed for years because their bleeding was ‘too quiet’ or ‘not bad enough.’ The part about angiodysplasia being mistaken for simple anemia? That’s heartbreaking. And the fact that some people have three negative scopes before being diagnosed? That’s a system failure. We need better training, better tools, and more compassion. This isn’t just about bleeding - it’s about being heard.