Therapeutic Drug Monitoring: What It Is and Why It Saves Lives
When you take a medication, your body doesn’t always process it the same way someone else does. That’s where therapeutic drug monitoring, the practice of measuring the amount of a drug in your bloodstream to ensure it’s in the safe and effective range. Also known as TDM, it’s not just for hospital patients—it’s used daily for people on antidepressants, seizure meds, heart drugs, and even antibiotics like vancomycin. Without it, you could be getting too little to work—or too much and risking serious side effects.
Think of it like driving a car with no fuel gauge. You might make it to the next gas station, or you might run out in the middle of nowhere. blood tests, the core tool used in therapeutic drug monitoring to measure drug concentration give doctors that gauge. They check levels at specific times—after a dose, before the next one—to see if your body is absorbing, breaking down, or clearing the drug the way it should. For example, someone on lithium for bipolar disorder needs regular tests because the difference between a helpful dose and a toxic one is tiny. Same goes for dosage adjustment, the process of changing a medication amount based on blood test results to optimize treatment. It’s not about sticking to a standard prescription—it’s about personalizing it.
Many of the posts here tie directly into this. You’ll find stories about how mixing sedating drugs can lead to respiratory failure, how opioids lower testosterone, or how expired antibiotics lose potency. All of these are risks that therapeutic drug monitoring can help prevent. If your doctor doesn’t check your drug levels, you’re flying blind. That’s why this isn’t just a lab procedure—it’s a safety net. Whether you’re on a high-risk medication, have kidney or liver issues, or are taking multiple drugs at once, knowing your actual drug levels can mean the difference between feeling better and ending up in the ER.
Below, you’ll find real cases where people learned the hard way what happens when drug levels aren’t tracked—like dangerous interactions between cannabis and blood thinners, or how goldenseal can mess with diabetes meds. These aren’t hypotheticals. They’re everyday risks. And therapeutic drug monitoring is the tool that turns guesswork into control.
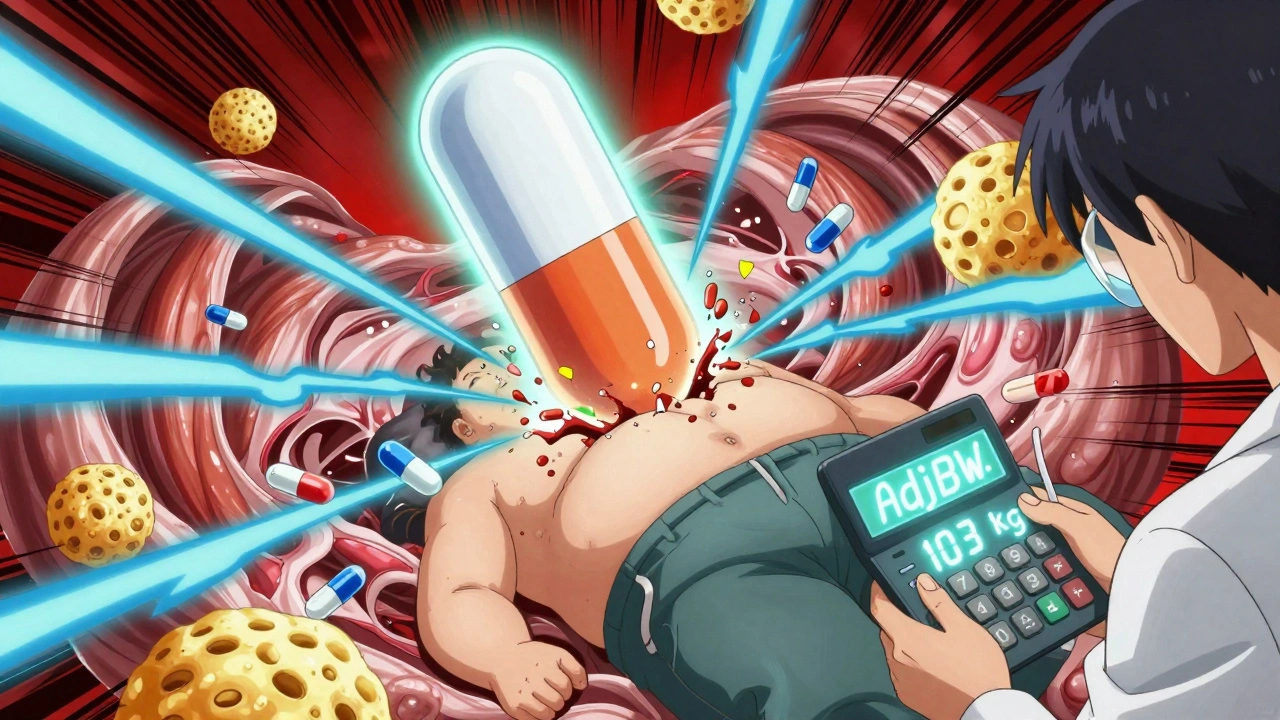
Obesity changes how drugs move through your body - standard doses often fail. Learn how lean body weight, adjusted dosing, and therapeutic monitoring prevent treatment failure and toxicity in obese patients.