Hospital to Home Transition: What You Need to Know About Medication Safety and Care Coordination
When you leave the hospital, your care doesn’t end—it just moves. The hospital to home transition, the period when patients move from inpatient care to managing their health at home. Also known as discharge planning, it’s one of the most dangerous moments in modern healthcare, where mistakes can send you right back in. Studies show nearly 1 in 5 Medicare patients ends up back in the hospital within 30 days after discharge, and medication errors are the #1 cause.
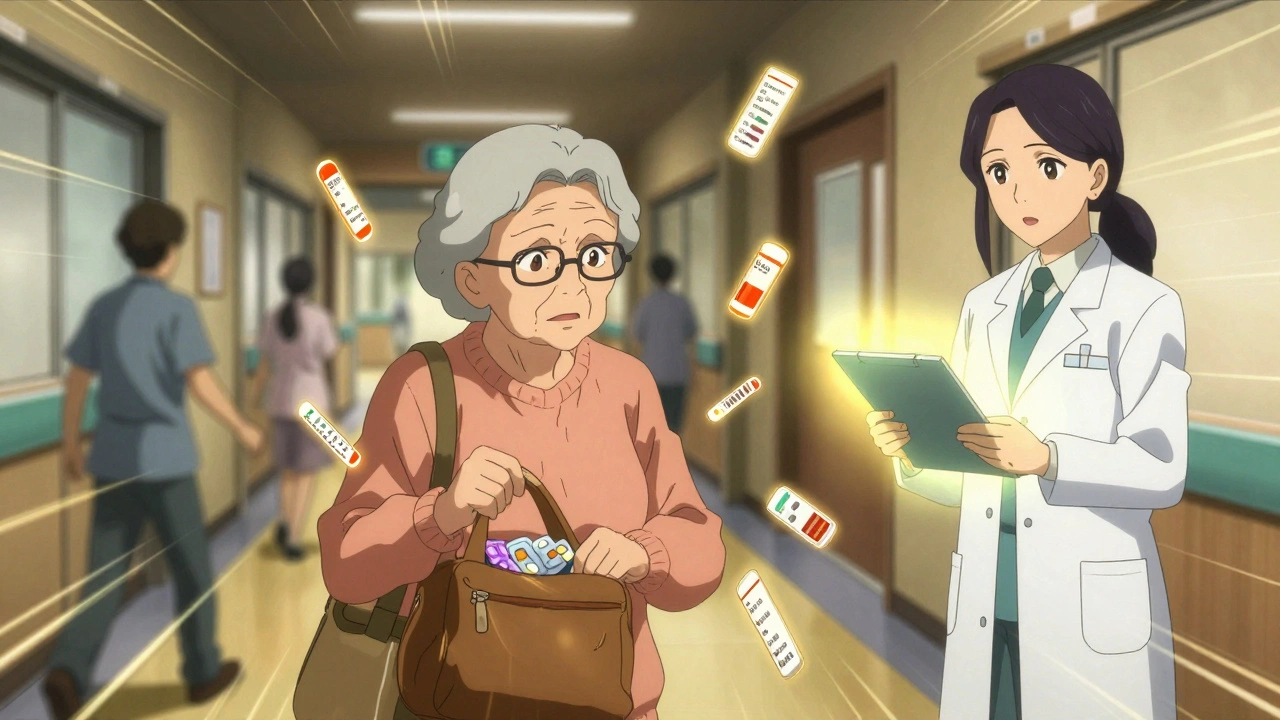
This isn’t just about picking up prescriptions. It’s about medication safety, the practice of ensuring drugs are taken correctly, without harmful interactions or gaps. Think about it: you’re often sent home with 5, 10, even 15 new or changed meds. Some you’ve never heard of. Some you’re told to stop. Others you’re told to start—right away. Without clear instructions, it’s easy to mix up doses, skip pills, or combine something dangerous like alcohol with your new painkiller. That’s why care coordination, the process of making sure all your doctors, pharmacists, and family are on the same page matters more than the discharge paperwork itself.
And it’s not just seniors. Anyone coming out of surgery, a heart event, or a serious infection is at risk. You might think your doctor explained everything, but in a 10-minute discharge chat, details get lost. That’s why medication adherence, how well you actually follow your drug schedule is the real test—not whether you left the hospital with a pill bottle in hand. Many patients don’t know why they’re taking a drug, what it’s for, or what happens if they miss a dose. And if you’re on something like an MAO inhibitor, opioids, or blood thinners, getting it wrong can be deadly.
The good news? You don’t have to figure this out alone. The posts below cover exactly what goes wrong—and what works. You’ll find how to sync your refills so you never run out, how to spot overdose signs before it’s too late, why some meds don’t work right after you gain or lose weight, and how to talk to your pharmacist about costs and interactions. You’ll learn how to handle sharps safely if you’re on injections, how to avoid deadly combos like alcohol and sedatives, and why even natural supplements can mess with your prescriptions. This isn’t theory. These are real situations people face every day after leaving the hospital.
If you or someone you love is heading home after a hospital stay, this collection gives you the tools to make sure you don’t fall through the cracks. The system isn’t perfect—but you can be smarter than it.
Learn how to prevent dangerous medication errors when leaving the hospital, especially for seniors on multiple drugs. Key steps include pharmacist-led reconciliation, the Teach-Back method, and follow-up within 7 days.