When a child develops Deep Vein Thrombosis in Children is a blood clot that forms in a deep vein, most often in the leg, and can threaten a youngster’s health if not spotted early. While adult DVT gets most of the headlines, paediatric cases have distinct triggers, warning signs, and treatment pathways. This guide walks you through the why, what, and how so you can act fast if you suspect a clot in a child.
Quick Facts
- Incidence: roughly 0.07 cases per 1,000 hospitalized children.
- Common sites: femoral, popliteal, and iliac veins.
- Top risk factors: central venous catheters, inherited clotting disorders, immobility.
- First‑line imaging: compression ultrasound (Doppler).
- Treatment duration: usually 3-6 months, longer if an underlying thrombophilia exists.
What Exactly Is a Blood Clot in a Kid?
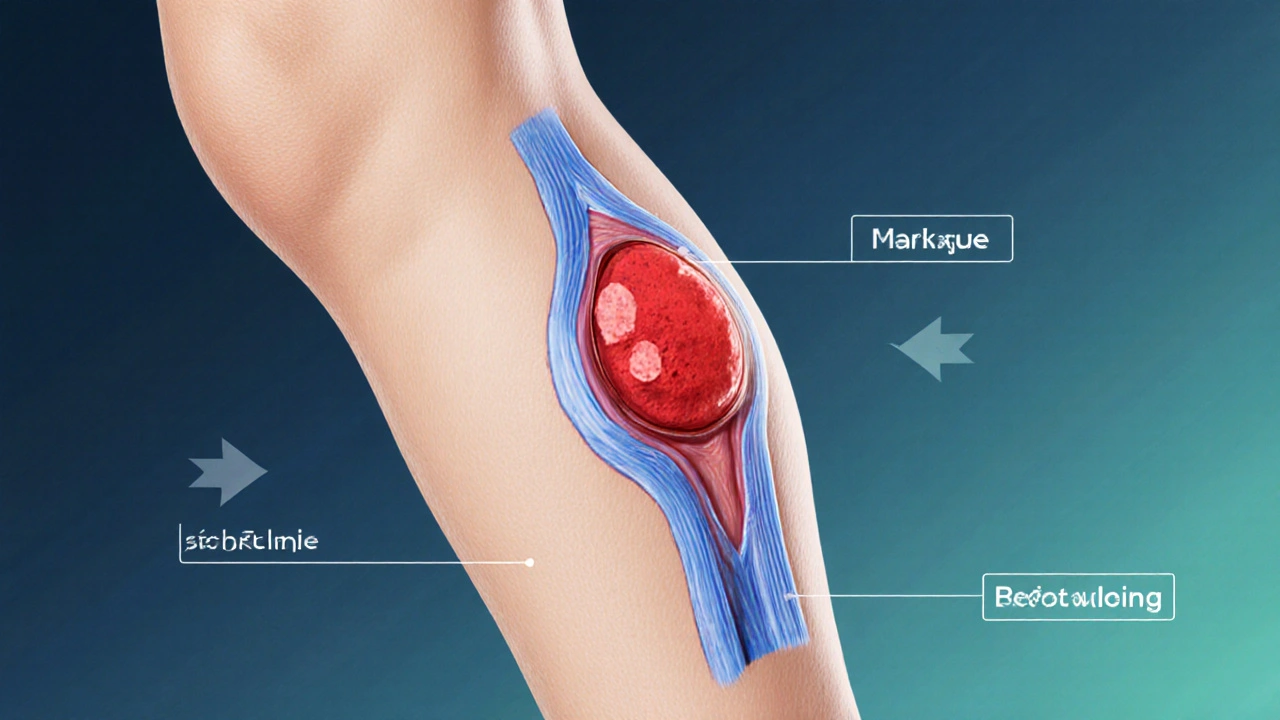
A blood clot (or thrombus) is a gel‑like mass of fibrin, platelets, and trapped red blood cells that blocks normal blood flow. In children, the clot usually forms in a deep vein of the lower limb but can appear in the arm, neck, or even the brain’s venous sinuses. Because the clot sits away from the skin’s surface, it’s easy to miss until swelling, pain, or a serious complication like a pulmonary embolism occurs.
Main Causes and Risk Factors
Unlike adults, where lifestyle factors dominate, paediatric DVT often stems from medical or genetic triggers. Below are the most frequently seen causes:
- Central venous catheter (CVC): The tube provides a direct pathway for clot formation. Up to 40% of hospital‑acquired DVTs involve a CVC.
- Inherited thrombophilia: Mutations such as Factor V Leiden or prothrombin G20210A increase clot risk by 2-4×.
- Immobilization: After surgery, severe illness, or prolonged bed rest, venous stasis can set the stage for clotting.
- Obesity: Excess weight adds pressure on the veins and promotes a pro‑coagulant state.
- Trauma or fracture: Damage to vessels releases tissue factor, kicking off the clotting cascade.
- Infection and inflammation: Sepsis or inflammatory bowel disease raise clotting factors in the blood.
- Cancer therapy: Certain chemotherapeutic agents and radiation damage the endothelium, making clots more likely.
Spotting the Signs: Symptoms Parents Should Watch For
Kids can’t always articulate what’s wrong, so look for physical clues:
- Unexplained swelling in a leg or arm, often asymmetrical.
- Warmth and redness over the affected area.
- Sharp or throbbing pain that worsens with movement.
- Visible dilated veins near the skin.
- Shortness of breath, rapid heartbeat, or chest pain - possible warning of a pulmonary embolism.
Even mild symptoms deserve prompt medical attention because paediatric clots can progress quickly.
How Doctors Diagnose a Pediatric DVT
The diagnostic work‑up balances thoroughness with a child’s tolerance for tests.
- Clinical assessment: A careful history (recent surgery, catheter use) and physical exam set the stage.
- Compression ultrasound with Doppler: First‑line, non‑invasive, and highly sensitive for lower‑limb clots.
- Magnetic Resonance Venography (MRV): Used when ultrasound is inconclusive, especially for pelvic or central veins.
- Laboratory tests: D‑dimer levels can help rule out clotting; a coagulation panel screens for inherited disorders.
- Chest CT angiography: Reserved for cases where a pulmonary embolism is suspected.
Treatment Options: From Anticoagulants to Compression
Once a clot is confirmed, the goal is to stop it from growing, prevent new clots, and reduce the risk of embolism. The treatment plan depends on clot size, location, and the child’s overall health.
Anticoagulant Therapy
Anticoagulants thin the blood, allowing the clot to dissolve naturally. Below is a quick comparison of the most common agents used in paediatrics.
| Drug | Administration | Typical Dose | Monitoring Needed | Notes |
|---|---|---|---|---|
| Unfractionated Heparin | IV infusion | 15‑25U/kg/hr | aPTT every 6h | Rapid onset, reversible with protamine. |
| Low‑Molecular‑Weight Heparin (LMWH) | Sub‑Q injection | 1mg/kg bid | Anti‑Xa level 0.5‑1.0IU/mL | Preferred for outpatient care. |
| Warfarin | Oral | 0.1‑0.2mg/kg daily | INR 2‑3 weekly | Long‑term use, many drug interactions. |
| Direct Oral Anticoagulants (DOACs) | Oral | Weight‑based dose per product | No routine labs needed | Emerging data; approved for adolescents ≥12y. |
For most children, LMWH is the first choice because it can be given at home and requires less frequent blood draws.
Adjunct Therapies
- Compression stockings: Graduated pressure improves venous return, reduces swelling, and lowers recurrence risk.
- Thrombolysis: Reserved for massive clots threatening limb viability; involves catheter‑directed delivery of tissue plasminogen activator (tPA).
- Mechanical thrombectomy: Rare, used when clot burden is very high and anticoagulation alone isn’t enough.
Duration of Therapy
Standard treatment lasts 3months for a provoked clot (e.g., post‑surgery). If an inherited thrombophilia or unprovoked clot is identified, clinicians often extend therapy to 6-12months and may consider lifelong prophylaxis in high‑risk scenarios.
Managing Complications and Follow‑Up Care
Even after the clot resolves, children can face lingering issues:
- Post‑thrombotic syndrome: Chronic pain, swelling, and skin changes. Early physiotherapy and compression help.
- Recurrent DVT: Follow‑up duplex ultrasound at 1, 3, and 6months monitors for new clots.
- Pulmonary embolism (PE): Any sudden chest pain or breathing difficulty warrants immediate imaging.
Family education is critical. Parents should know the signs of recurrence and maintain a schedule for medication refills and imaging appointments.
Prevention: What Parents and Caregivers Can Do
Preventing a clot is often about minimizing known triggers:
- Limit catheter time: Remove CVCs as soon as they’re no longer medically necessary.
- Encourage movement: Even short walks after surgery lower venous stasis.
- Maintain a healthy weight: Balanced diet and regular activity keep clotting factors in check.
- Screen for inherited risks: If a close family member had a clot, ask the pediatrician about genetic testing.
- Hydration: Adequate fluid intake keeps blood less viscous.
In high‑risk settings, some doctors prescribe low‑dose aspirin or prophylactic LMWH, but that decision always rests on a thorough risk‑benefit analysis.

Frequently Asked Questions
Can a child’s DVT heal without medication?
Mild clots sometimes resolve with just compression and early mobilisation, but most paediatric DVTs need anticoagulation to prevent propagation and pulmonary embolism. Skipping medication puts the child at serious risk.
Is ultrasound painful for a child?
No. The probe glides over the skin with a water‑based gel. It’s painless and usually takes 15‑20 minutes.
How long does anticoagulation therapy last?
For a clot linked to a clear trigger, 3months is typical. If the clot is unprovoked or the child has a clotting disorder, treatment often extends to 6months or longer.
Are DOACs safe for kids under 12?
Most DOACs are approved only for adolescents 12years and older. Ongoing trials are evaluating safety in younger children, but currently the standard of care remains LMWH or unfractionated heparin.
What is the chance of a second clot?
Recurrence rates hover around 10‑15% within one year for children with a known thrombophilia, versus 2‑3% for those with a single, provoked event.
Understanding the unique facets of paediatric deep vein thrombosis empowers families to act swiftly, collaborate closely with healthcare teams, and reduce the odds of long‑term complications. If you suspect any of the warning signs, seek medical attention right away-early diagnosis can make all the difference.



Katherine Krucker Merkle
September 28 2025Wow, that’s a solid rundown of pediatric DVT – I didn’t realize how common central lines are as a trigger. It’s reassuring to see the emphasis on early ultrasound since kids can’t always tell us what’s wrong. The section on compression stockings feels practical, especially for families trying to manage at home. Thanks for pulling together the risk factors and treatment options in one place.
Mark Quintana
October 7 2025this info is supar helpful
Brandon Cassidy
October 16 2025Reading through the guide, I’m struck by how the pediatric approach mirrors adult protocols yet diverges in nuance. The reliance on LMWH for outpatient care reflects a balance between efficacy and child‑friendly administration. It also underscores the importance of tailoring anticoagulation duration to the underlying etiology, which is a principle that resonates across age groups. The discussion of post‑thrombotic syndrome reminds us that the story doesn’t end with clot resolution. Overall, the piece stitches together pathophysiology and practical steps in a clear manner.
Taylor Yokum
October 25 2025Exactly! LMWH is like the Goldilocks of blood thinners – not too heavy, not too light, just right for kids.
Taryn Esses
November 4 2025Good to know that ultrasound isn’t painful; that makes it easier to get kids on board.
Albert Lopez
November 13 2025The presented overview, while comprehensive, falls short in its critical appraisal of the evidence base underpinning pediatric anticoagulation regimens. First, the reliance on low‑molecular‑weight heparin as the default therapy is predicated on convenience rather than a robust comparative effectiveness analysis against unfractionated heparin or emerging direct oral anticoagulants. Second, the cited incidence of 0.07 cases per 1,000 admissions lacks stratification by underlying comorbidities, obscuring the true burden among high‑risk cohorts such as oncology patients. Third, the discussion of inherited thrombophilia does not address the variable penetrance of Factor V Leiden heterozygosity, which can lead to over‑treatment in marginal cases. Fourth, the recommendation for a three‑month treatment duration for provoked clots is presented as a blanket guideline, yet recent multicenter trials suggest that shorter courses may be non‑inferior in select circumstances. Fifth, the omission of cost‑effectiveness considerations for long‑term LMWH supplies neglects a pivotal factor in health‑system decision‑making. Sixth, the brief mention of compression stockings fails to acknowledge the paucity of pediatric‑specific data on adherence and efficacy. Seventh, the algorithmic approach to diagnostic imaging does not contemplate the radiation exposure associated with repeated CT angiography in the context of suspected pulmonary embolism. Eighth, the article does not explore the potential role of point‑of‑care ultrasound as a bedside screening tool, which could accelerate diagnosis in resource‑limited settings. Ninth, the lack of a structured follow‑up protocol beyond duplex ultrasound at six months leaves clinicians without guidance on monitoring for late sequelae such as post‑thrombotic syndrome. Tenth, the brief FAQ section glosses over the nuanced decision‑making required when considering prophylactic anticoagulation in children with indwelling catheters. In sum, while the guide serves as a useful primer, it would benefit from a more rigorous interrogation of the primary literature and a clearer articulation of the uncertainties that persist in pediatric venous thromboembolism management. Moreover, future research should prioritize randomized controlled trials comparing DOACs to LMWH in the pediatric population, as current data remain anecdotal. Additionally, interdisciplinary teams involving hematology, radiology, and nursing should develop standardized pathways to reduce practice variation. Finally, parental education materials must be culturally sensitive and accessible to ensure adherence across diverse communities. Only through such systematic enhancements can we transition from a descriptive guide to an evidence‑driven standard of care.
Halle Redick
November 22 2025Great job breaking down a scary topic into bite‑size pieces – parents will feel a lot less overwhelmed now!
Erica Harrington
December 1 2025Exactly, the more we demystify these medical details, the more families can act confidently and keep their kids moving forward.
Patricia Mombourquette
December 11 2025DVT in kids is rare but serious. Parents need to watch for swelling and pain. Ask doc ASAP
karl lewis
December 20 2025While the article is thorough, it neglects recent pharmacokinetic data on pediatric DOACs, which could inform safer dosing strategies. 🧐