Obesity Medication Dosing: Safe Amounts, Risks, and What Works
When it comes to obesity medication dosing, the precise amount of weight-loss drugs prescribed to manage excess body weight based on individual health needs and response. Also known as anti-obesity drug dosing, it’s not just about popping a pill—it’s about matching the right dose to your body, your health history, and your goals. Too little and you won’t see results. Too much and you risk serious side effects like nausea, rapid heartbeat, or even pancreatitis. Unlike antibiotics or painkillers, these medications are tuned slowly, often starting at a low dose and creeping up over weeks to let your body adjust.
Semaglutide, a GLP-1 receptor agonist used for chronic weight management and type 2 diabetes. Also known as Wegovy, it is commonly prescribed at 0.25 mg weekly, then increased every four weeks up to 2.4 mg. Many people don’t realize that skipping a dose or doubling up can throw off your metabolism and trigger vomiting or dizziness. Liraglutide, another GLP-1 drug sold as Saxenda, follows a similar ramp-up pattern, starting at 0.6 mg and increasing to 3.0 mg daily. Also known as Saxenda, it requires daily injections and strict timing with meals to avoid blood sugar crashes. These drugs don’t work like stimulants—they’re slow-acting, hormone-based tools that reduce appetite and slow digestion. That’s why sticking to the schedule matters more than you think.
Obesity medication dosing also depends on what else you’re taking. If you’re on insulin, blood pressure meds, or even supplements like St. John’s wort, your doctor needs to know. Some drugs can interfere with absorption or amplify side effects. For example, combining semaglutide with other sedating medications can increase drowsiness, while certain antibiotics might reduce how well your body processes the weight-loss drug. Even alcohol can mess with your tolerance and make nausea worse. It’s not just about the pill—it’s about your whole health picture.
And dosing isn’t static. If you lose weight, your dose might need adjusting. If you develop new health issues—like kidney trouble or gallbladder disease—your doctor may lower or stop the medication. Many people assume once they start, they’re locked in. But these drugs are tools, not life sentences. Some people stay on them for years. Others taper off after hitting their goal, especially if they’ve built better habits around food and movement.
What you’ll find below are real stories and facts from people who’ve been there. Posts cover what happens when doses go wrong, how to spot early signs of overdose, why some people don’t respond even at full dose, and how to talk to your pharmacist about timing and refills. You’ll see how drug interactions, like those with opioids or thyroid meds, can change everything. No fluff. No marketing. Just what works, what doesn’t, and what you need to ask before you start—or keep taking—these medications.
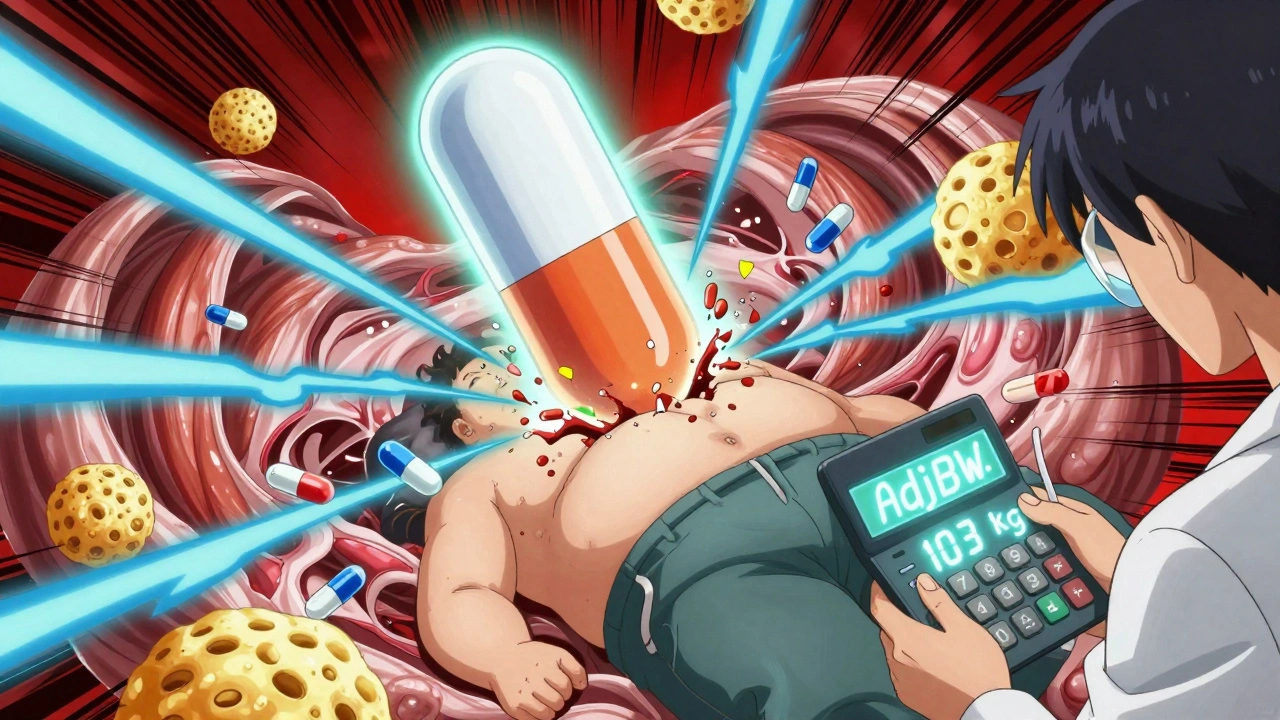
Obesity changes how drugs move through your body - standard doses often fail. Learn how lean body weight, adjusted dosing, and therapeutic monitoring prevent treatment failure and toxicity in obese patients.