Medication Reconciliation: Why It Saves Lives and How It Works
When you're taking multiple drugs, medication reconciliation, the process of comparing your current medications with what you should be taking to avoid errors and harmful interactions. It's not just paperwork—it’s a safety net. Think of it like checking your GPS before a road trip. If your phone says you’re heading to Boston but your map says Maine, you stop and fix it. Your meds work the same way. A simple mismatch—a forgotten blood thinner, a duplicate dose of painkillers, or a new antibiotic clashing with your heart pill—can land you in the ER.
This isn’t theoretical. A 2023 study in the Journal of Patient Safety found that over 70% of medication errors in hospitals happened because no one checked what the patient was actually taking at home. drug interactions, when two or more medications change each other’s effects are the silent killers here. You might not feel anything until your liver fails, your blood pressure spikes, or your breathing slows. That’s why medication safety, the practice of preventing harm from medicines through clear communication and verification starts with a list. Not a memory. Not a pill bottle. A written, updated, verified list.
It’s not just for hospitals. If you see three doctors, fill prescriptions at two pharmacies, or take supplements on top of your pills, you’re at risk. pharmacy refills, the process of getting more of your prescribed drugs can become a minefield if they’re not synced. One pharmacy gives you a new blood pressure med. Another keeps refilling an old one you stopped. You don’t know which is active. That’s where medication adherence, how well you take your drugs exactly as prescribed meets real-world chaos. People forget. They run out. They skip doses because of cost. Then they restart—and no one knows what’s going on.
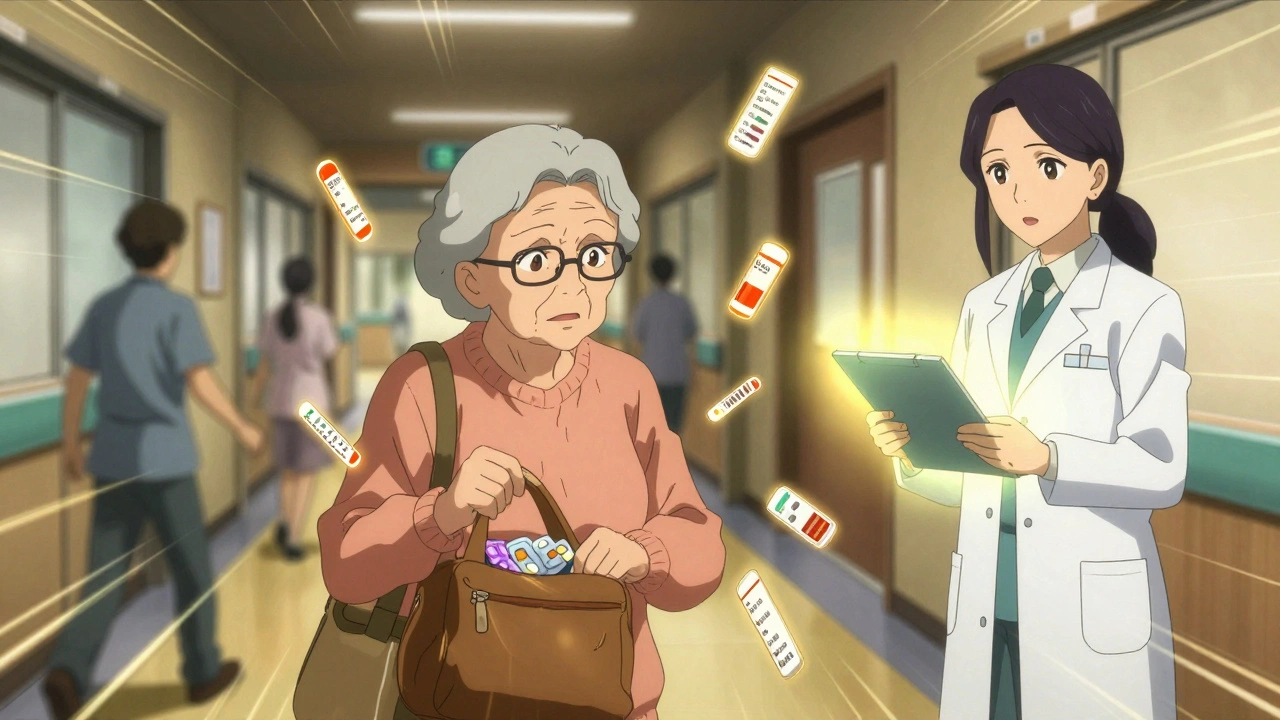
Medication reconciliation fixes that. It’s a conversation. With your doctor. With your pharmacist. Sometimes with your family. You bring your pills in a bag—not a list. They compare it to what’s on paper. They ask: Are you still taking this? Did your pain doctor change your dose? Did you start turmeric for inflammation? That’s when they catch the goldenseal messing with your metformin, or the alcohol making your sedatives deadly. It’s not glamorous. But it’s life-saving.
You don’t need to be sick to need this. If you’re on five or more meds, or if you’ve been hospitalized in the last year, you’re a prime candidate. Even if you think you know your own meds, you don’t. Not really. Not unless you’ve sat down with someone who’s holding your actual pill bottles and asking you why you stopped the beta-blocker last month. That’s the moment mistakes get caught.
The posts below cover the real-world fallout of skipped reconciliations: deadly drug combos, how opioids lower testosterone, why expired antibiotics fail, how cannabis messes with liver enzymes, and why generics sometimes feel different—even when they’re chemically identical. You’ll find guides on syncing refills, spotting overdose signs, and talking to your doctor about costs. This isn’t theory. It’s what happens when the system breaks—and how to keep it from breaking on you.
Learn how to prevent dangerous medication errors when leaving the hospital, especially for seniors on multiple drugs. Key steps include pharmacist-led reconciliation, the Teach-Back method, and follow-up within 7 days.