Medication Errors: What They Are, How They Happen, and How to Prevent Them
When you take a pill, you expect it to help—not hurt. But medication errors, mistakes in prescribing, dispensing, or taking drugs that lead to harm. Also known as drug errors, they’re one of the leading causes of preventable injury in healthcare. These aren’t just rare accidents. They happen every day because of simple oversights: a confusing label, a missed refill, or mixing alcohol with a prescription. And they’re not always your fault. A pharmacist might misread a script. A doctor might not know you’re taking another drug. Even the way your body processes medicine can turn a safe dose into a dangerous one.
One big reason medication errors happen is because of drug interactions, when two or more medications change each other’s effects in the body. This isn’t just about pills clashing—it’s about how alcohol, herbs, or even grapefruit juice can turn a normal dose into a life-threatening one. For example, mixing MAO inhibitors with certain foods or cold medicines can cause a sudden spike in blood pressure. Or combining sedatives like opioids and benzodiazepines can slow your breathing to a stop. These aren’t theoretical risks. They’re documented in real cases, and they happen to people just like you. Another major issue is medication adherence, how well patients take their drugs exactly as prescribed. If you skip doses, take them at the wrong time, or stop because they cost too much, you’re not just wasting money—you’re risking serious health setbacks. Gaps in therapy can make chronic conditions worse, and in older adults, even a single missed dose of a blood thinner or diabetes drug can land you in the hospital. Then there’s overdose signs, the early warning signals that something’s gone wrong with your medication. These aren’t always obvious. A slow heartbeat, confusion, extreme drowsiness, or sudden nausea might not seem like an emergency—but they could be the first signs of an overdose. Knowing these signals can save your life or someone else’s.
What’s clear is that medication errors aren’t about being careless. They’re about systems that are too complex, information that’s hard to find, and costs that force impossible choices. The good news? You don’t have to accept this as normal. You can ask questions. You can check your prescriptions against your list of meds. You can use tools like medication synchronization to avoid gaps. And you can learn what combinations to avoid—like alcohol with painkillers, or goldenseal with metformin. The posts below give you real, practical advice on how to spot these mistakes before they happen, how to talk to your doctor about risks, and what to do if something feels off. This isn’t theory. It’s what keeps people safe.
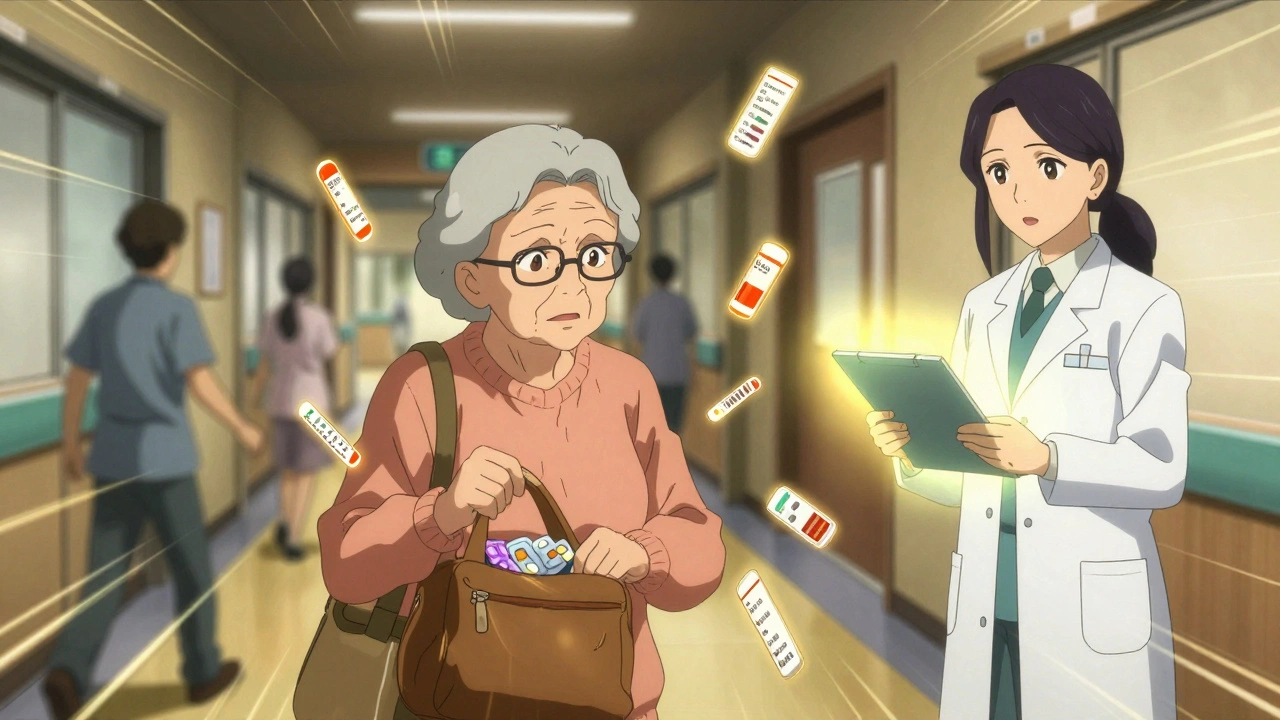
Learn how to prevent dangerous medication errors when leaving the hospital, especially for seniors on multiple drugs. Key steps include pharmacist-led reconciliation, the Teach-Back method, and follow-up within 7 days.