BMI and Drug Levels: How Body Weight Affects Medication Effectiveness
When you take a pill, your body doesn’t treat everyone the same. BMI, a number that estimates body fat based on height and weight. Also known as body mass index, it’s not just a number on a scale—it directly affects how drugs move through your system. A higher BMI can mean drugs stay in your system longer, get absorbed slower, or don’t reach the right concentration to work properly. This isn’t theory—it’s why some people feel their meds aren’t working, even when they take them exactly as prescribed.
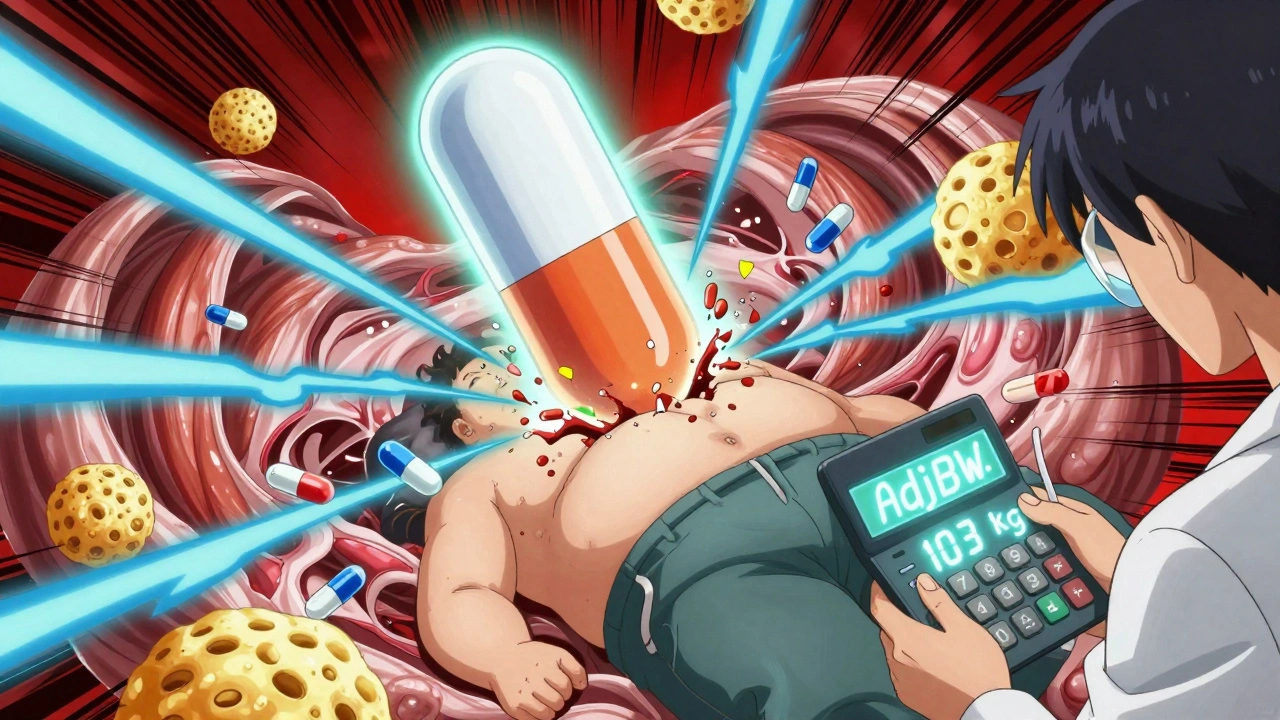
Drug metabolism, how your liver and kidneys break down and remove medications changes with body composition. Fat tissue doesn’t just sit there—it actively holds onto certain drugs, especially ones that dissolve in fat. That means someone with a higher BMI might need a bigger dose for the same effect. On the flip side, water-soluble drugs like some antibiotics or diuretics spread differently in leaner bodies, making standard doses too strong for smaller people. Medication dosing, the amount and frequency of a drug given to a patient isn’t one-size-fits-all. Studies show that for drugs like opioids, antidepressants, and blood thinners, dosing based on actual weight leads to better results and fewer side effects than using a flat dose for everyone.
It’s not just about getting the right dose. Pharmacokinetics, how the body absorbs, distributes, metabolizes, and excretes a drug shifts with body fat, liver function, and even kidney health—all of which tie back to BMI. Someone with obesity might process a drug slower, leading to buildup and toxicity. Someone underweight might clear it too fast, making the drug useless. This is why doctors sometimes check blood levels of certain meds, especially for epilepsy drugs, heart medications, or psychiatric treatments. It’s not paranoia—it’s precision.
You won’t always hear about this. Most prescriptions come with a standard dose printed on the bottle. But if you’ve ever felt your medication didn’t work right, or if you’ve had side effects others didn’t, your BMI might be part of the story. It’s not about blame—it’s about biology. The same drug can be life-saving for one person and dangerous for another, simply because of how their body is built.
Below, you’ll find real cases where body weight changed everything—from opioid side effects to how antidepressants work, and why some meds fail silently in people with higher BMI. These aren’t hypotheticals. They’re stories of people who thought they were doing everything right—until they learned the truth about how their body handled the drugs.
Obesity changes how drugs move through your body - standard doses often fail. Learn how lean body weight, adjusted dosing, and therapeutic monitoring prevent treatment failure and toxicity in obese patients.